Atrophic Gastroenteritis: Causes, Symptoms & Treatment Guide
 Oct, 21 2025
Oct, 21 2025
Atrophic Gastroenteritis Nutrient Deficiency Assessment Tool
This tool helps identify potential nutrient deficiencies associated with atrophic gastroenteritis based on your symptoms. Select the symptoms you're experiencing to receive personalized guidance on possible deficiencies and next steps.
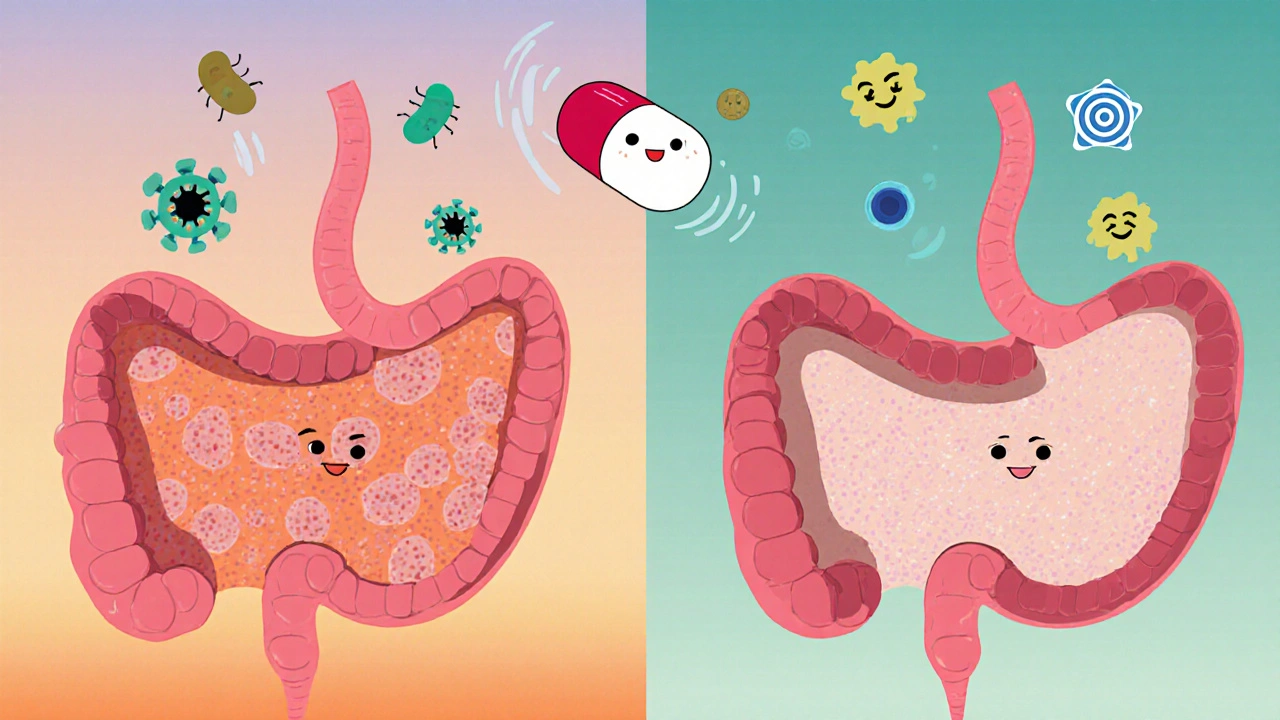
Atrophic gastroenteritis is a chronic inflammation of the stomach lining that leads to the loss of gastric glandular cells. When these cells disappear, the stomach can’t produce enough acid or intrinsic factor, paving the way for nutrient deficiencies and a range of digestive problems.
What Triggers Atrophic Gastroenteritis?
The condition rarely appears out of the blue. Several underlying mechanisms set the stage for the glandular loss:
- Autoimmune gastritis - the immune system attacks parietal cells, the very cells that make stomach acid and intrinsic factor.
- H. pylori infection - the bacterium causes chronic inflammation, and over years it can erode gastric glands.
- Long‑term use of proton pump inhibitors (PPIs) - suppressing acid for years may alter the stomach’s microbial balance and promote atrophy.
- Dietary factors, especially a diet low in B‑vitamins and iron, can worsen the loss of glandular tissue.
- Genetic predisposition - certain HLA types increase the risk of autoimmune attack on the stomach.
In many patients, more than one trigger overlaps, making the disease harder to pinpoint.
How to Spot the Symptoms
Because the stomach’s acid output drops, the classic burning pain of gastritis often fades. Instead, people notice subtler signs:
- Persistent fatigue - often due to vitamin B12 deficiency or iron deficiency anemia.
- Glossy, sore tongue and mouth ulcers - classic clues of B12 shortage.
- Unexplained weight loss or early satiety - the stomach can’t signal hunger properly.
- Frequent bloating, belching, or a feeling of fullness after a small meal.
- Nausea or occasional vomiting, sometimes with a metallic taste.
- Neurological tingling or numbness in the hands and feet - a later sign of severe B12 malabsorption.
Symptoms often develop slowly, so many patients don’t recognize the pattern until blood tests reveal deficiencies.
Diagnosing Atrophic Gastroenteritis
A solid diagnosis blends history, labs, and visual inspection of the lining:
- Blood work - check for low hemoglobin, low serum B12, low ferritin, and the presence of anti‑parietal cell antibodies.
- Upper endoscopy - using an endoscope, doctors visually assess the mucosa. Atrophic areas appear pale, thin, and less vascular.
- Biopsy - tiny tissue samples taken during endoscopy are examined under histopathology. Pathologists look for loss of oxyntic glands, intestinal metaplasia, and inflammatory infiltrates.
- Urea breath test or stool antigen test - to rule in or out current H. pylori infection.
When the biopsy shows extensive glandular loss with intestinal metaplasia, the diagnosis of atrophic gastroenteritis is usually confirmed.

Treatment Roadmap
Treatment focuses on three pillars: eliminating the underlying cause, correcting nutrient gaps, and protecting the remaining gastric tissue.
1. Eradicate H. pylori (if present)
A standard triple‑therapy regimen-clarithromycin, amoxicillin (or metronidazole), and a PPI for 14 days-cures the bacterium in about 85‑90 % of cases. Follow‑up testing ensures success.
2. Manage Autoimmune Attack
There’s no cure for the autoimmune process, but you can limit damage:
- Stop unnecessary long‑term PPIs; discuss alternative reflux management with your doctor.
- Vaccinate against common pathogens; infections can trigger flare‑ups.
- In rare severe cases, low‑dose steroids or immunomodulators may be prescribed.
3. Replace Missing Nutrients
Because the stomach can’t absorb B12 or iron efficiently, oral supplements often fall short.
- Vitamin B12 - intramuscular injections (1000 µg weekly for four weeks, then monthly) or high‑dose sublingual tablets (1000 µg daily) are effective.
- Iron - intravenous iron sucrose or ferric carboxymaltose bypasses the gut’s reduced absorption.
- Multivitamin formulas enriched with folate, calcium, and vitamin D support overall health.
4. Surveillance for Cancer
Chronic atrophy can progress to intestinal metaplasia and eventually gastric adenocarcinoma. Guidelines recommend:
- Endoscopic surveillance every 3 years if metaplasia is present.
- More frequent checks (every 1‑2 years) for patients with a family history of gastric cancer.
5. Lifestyle Tweaks
While lifestyle changes won’t reverse atrophy, they can reduce symptom burden:
- Eat small, frequent meals; avoid overly spicy or acidic foods.
- Stay hydrated but limit coffee and carbonated drinks that may irritate the lining.
- Quit smoking; nicotine impairs mucosal healing.
- Maintain a balanced diet rich in lean protein, leafy greens, and fortified cereals to support nutrient intake.
Comparing Atrophic Gastroenteritis with Other Chronic Gastritis Types
| Feature | Atrophic Gastroenteritis | Autoimmune Gastritis | H. pylori‑Associated Gastritis |
|---|---|---|---|
| Primary Cause | Combination of autoimmune and H. pylori factors, long‑term acid suppression | Auto‑antibodies against parietal cells | Chronic infection with Helicobacter pylori |
| Typical Age | 50‑70 years | Middle‑aged to elderly | Often diagnosed in younger adults (30‑50 years) |
| Glandular Loss | Marked atrophy of oxyntic glands | Severe parietal cell loss | Variable; may progress to atrophy after years |
| Associated Deficiencies | Vitamin B12, iron, folate | Vitamin B12 only | Iron (via chronic bleeding), sometimes B12 |
| Cancer Risk | Elevated (intestinal metaplasia → adenocarcinoma) | High (type I gastric carcinoid, adenocarcinoma) | Moderate; risk rises with atrophic change |

Frequently Asked Questions
Can atrophic gastroenteritis be reversed?
Complete reversal is rare because glandular cells are lost permanently. However, treating the underlying cause, stopping acid‑suppressing drugs, and correcting nutrient deficiencies can halt further damage and improve symptoms.
How long does it take for B12 injections to improve fatigue?
Most patients notice a boost in energy within 1‑2 weeks of the initial injection series, though full neurologic recovery may take several months.
Is a gluten‑free diet helpful?
Only if you have co‑existing celiac disease. For pure atrophic gastroenteritis, a gluten‑free diet offers no proven benefit.
What follow‑up schedule is recommended after treatment?
After eradication of H. pylori and nutrient replacement, an endoscopic check every 3 years is standard. Blood work to monitor B12 and iron should be done every 6‑12 months.
Can children develop atrophic gastroenteritis?
It’s uncommon, but pediatric cases linked to severe H. pylori infection or early‑onset autoimmune disorders have been reported.
Bottom Line
Understanding atrophic gastroenteritis means recognizing the silent loss of stomach glands, the nutrient gaps it creates, and the long‑term cancer risk. Early testing, targeted eradication of H. pylori, and aggressive vitamin B12/iron replacement can keep you feeling better and prevent complications. If you notice chronic fatigue, unexplained anemia, or persistent stomach upset, ask your doctor for a full work‑up-catching the disease early makes a huge difference.
erica fenty
October 21, 2025 AT 15:09The hallmark of atrophic gastroenteritis is B12 malabsorption, so monitor serum B12 and consider intramuscular injections early!
Ericka Suarez
October 23, 2025 AT 00:29THIS IS A DISASTER!!! If you keep ignoring it, your body will turn to rubble.
parbat parbatzapada
October 24, 2025 AT 09:49They dont tell you that long‑term PPI use is part of a hidden agenda to keep us dependent on pharmaceuticals. The industry pushes these pills while quietly starving our stomachs of acid. Its no coincidence that atrophy rates climb as prescriptions skyrocket.
Casey Cloud
October 25, 2025 AT 19:09Diagnosing atrophic gastroenteritis starts with a thorough clinical history that highlights fatigue, glossitis, and early satiety.
Next, a complete blood panel should include hemoglobin, ferritin, serum B12, and anti‑parietal cell antibodies to flag deficiencies and autoimmune activity.
If labs suggest a problem, an upper endoscopy is the gold standard for visualizing the gastric mucosa and obtaining targeted biopsies.
Biopsy specimens allow the pathologist to assess glandular loss, intestinal metaplasia, and inflammatory infiltrates, which solidify the diagnosis.
Testing for Helicobacter pylori via urea breath test or stool antigen is essential, because eradication can halt further atrophic change.
Once the underlying cause is identified, treatment proceeds on three fronts: eliminating the trigger, replenishing nutrients, and protecting remaining tissue.
For H. pylori, a standard triple‑therapy regimen of clarithromycin, amoxicillin (or metronidazole), and a short course of a PPI achieves cure in the majority of patients.
Autoimmune cases require cessation of unnecessary long‑term PPIs and, in select severe cases, low‑dose steroids or immunomodulators may be considered.
Nutrient replacement is critical; intramuscular vitamin B12 injections bypass the dysfunctional gastric absorption pathway and typically raise serum levels within weeks.
Intravenous iron formulations such as iron sucrose or ferric carboxymaltose provide rapid repletion for iron‑deficient patients who cannot absorb oral iron efficiently.
Regular monitoring of B12, iron, and folate every six months helps gauge therapeutic response and adjust dosing as needed.
Because chronic atrophy raises gastric cancer risk, endoscopic surveillance every three years is recommended when metaplasia is present.
Patients with a family history of gastric carcinoma should consider more frequent endoscopic checks, ideally every one to two years.
Lifestyle modifications, including small frequent meals, avoidance of irritants like excessive coffee and alcohol, and smoking cessation, support mucosal healing.
Together, these strategies can stabilize the disease, alleviate symptoms, and reduce the long‑term risk of malignancy.
Rachel Valderrama
October 27, 2025 AT 03:29Oh great, another reminder to inject myself like a lab rat.
Brandy Eichberger
October 28, 2025 AT 12:49While the article covers the basics, a more nuanced approach to supplementation includes using methylcobalamin over cyanocobalamin for better neural uptake, and pairing oral iron with vitamin C to enhance absorption.
Eli Soler Caralt
October 29, 2025 AT 22:09In the grand tapestry of gastric health, each bite is a stitch; choose threads that fortify rather than fray 😊.
Eryn Wells
October 31, 2025 AT 07:29Remember that cultural foods can be allies; fortified cereals and lentil stews offer natural B‑12 precursors when paired with proper cooking methods.
Kathrynne Krause
November 1, 2025 AT 16:49You’ve got the power to turn this around-small dietary wins add up to big health victories!
Chirag Muthoo
November 3, 2025 AT 02:09In summary, atrophic gastroenteritis results from a confluence of autoimmune attack, chronic Helicobacter pylori infection, and iatrogenic acid suppression, leading to glandular loss and subsequent nutrient deficiencies. Accurate diagnosis relies on serological markers, endoscopic visualization, and histological confirmation. Management mandates eradication of H. pylori where present, cessation of unnecessary proton pump inhibitors, and parenteral replacement of vitamin B12 and iron. Ongoing surveillance is essential given the elevated risk of gastric adenocarcinoma. Patients should be counseled on lifestyle adjustments to support mucosal integrity.
Jasmina Redzepovic
November 4, 2025 AT 11:29Anyone who doubts the efficacy of intravenous iron is simply ignoring the overwhelming clinical evidence that oral preparations are insufficient in atrophic states-this is basic gastro‑medicine, not opinion.