Chronic Sinusitis: How Allergies, Infections, and Surgery Affect Your Sinuses
 Nov, 17 2025
Nov, 17 2025
For many people, a stuffy nose that won’t go away isn’t just annoying-it’s exhausting. If you’ve had nasal congestion, facial pressure, or a dull loss of smell for more than three months, you’re not just dealing with a bad cold. You might have chronic sinusitis, a condition that affects nearly 1 in 10 adults worldwide. Unlike a typical sinus infection that clears up in a week or two, chronic sinusitis sticks around, often despite antibiotics, decongestants, or home remedies. The truth? Most cases aren’t caused by bacteria. They’re driven by inflammation, allergies, or structural problems in your sinuses.
What Exactly Is Chronic Sinusitis?
Chronic sinusitis, also called chronic rhinosinusitis, isn’t one single problem. It’s a group of conditions where the lining of your sinuses stays swollen and inflamed for 12 weeks or longer, even with treatment. Your sinuses are air-filled spaces behind your forehead, cheeks, and eyes. When they’re healthy, they drain mucus naturally. When they’re inflamed, that drainage gets blocked. Mucus builds up. Bacteria may grow. Pressure builds. And you feel it-in your face, your head, your throat. The official diagnosis requires at least two of these symptoms for 12+ weeks: blocked nose, thick nasal discharge (clear or colored), facial pain or pressure, and reduced or lost sense of smell. Many people also feel fatigued, have a bad taste in their mouth from postnasal drip, or get frequent coughs. It’s not just "a cold that won’t leave." It’s a persistent inflammatory condition. There are three main subtypes:- Chronic sinusitis without nasal polyps - Most common. Inflammation is driven by allergies, irritants, or immune responses.
- Chronic sinusitis with nasal polyps - Soft, noncancerous growths inside the nose or sinuses. These block airflow and mucus flow. About 1 in 4 people with chronic sinusitis have them.
- Allergic fungal rhinosinusitis - A rare form where fungi trigger an allergic reaction in the sinuses. Often linked to asthma and nasal polyps.
Why Do Allergies Make It Worse?
If you have hay fever, eczema, or asthma, your risk of chronic sinusitis jumps by 2.5 times. Why? Because allergies and sinus inflammation share the same underlying mechanism: your immune system overreacts to harmless things like pollen, dust mites, or pet dander. That overreaction doesn’t just cause sneezing-it triggers swelling in the nasal passages and sinuses. In fact, people with asthma are 3 to 4 times more likely to develop chronic sinusitis. The inflammation doesn’t stay put in the lungs; it spreads upward. That’s why so many asthma patients struggle with persistent nasal symptoms-even when their breathing seems under control. Allergy testing can pinpoint triggers. Avoiding them helps, but it’s rarely enough. That’s why doctors start with nasal saline rinses and corticosteroid sprays. These don’t treat the allergy itself, but they calm the inflammation it causes. Fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) reduce swelling in 60-70% of patients after 4-8 weeks of daily use. Antihistamines like loratadine or cetirizine can help if allergies are the main driver. Studies show they cut symptoms by 45-60% in allergic patients. But they don’t fix the structural blockage or chronic swelling. That’s why they’re often used alongside sprays-not instead of them.Are Infections Really the Cause?
You might think a lingering sinus infection needs more antibiotics. But here’s the surprise: in most chronic cases, bacteria aren’t the main problem. About 70% of chronic sinusitis cases have no active bacterial infection. Even when bacteria like Streptococcus pneumoniae or Haemophilus influenzae are found, they’re often just hanging out in the mucus-not causing the inflammation. Antibiotics won’t fix that. That’s why guidelines from the American Academy of Allergy, Asthma & Immunology say antibiotics should only be used if there’s clear evidence of a bacterial flare-up-like sudden worsening of symptoms, fever, or thick yellow-green mucus after weeks of stable condition. Even then, they’re usually given for just 21-28 days. Long-term antibiotics? They don’t work. And they can lead to resistance or gut problems. Environmental irritants play a bigger role than most realize. Smoking or being around secondhand smoke increases your risk by 35%. Air pollution, strong perfumes, and even dry indoor air from heating systems can irritate the sinus lining and make inflammation worse.
When Medical Treatment Isn’t Enough
Most people improve with nasal rinses, steroid sprays, and avoiding triggers. But if symptoms persist after 12 weeks of consistent treatment, it’s time to consider surgery. The gold standard is Functional Endoscopic Sinus Surgery (FESS). It’s not the dramatic procedure people imagine. No cutting through the face. No big scars. Instead, a thin camera (endoscope) is inserted through the nostril. The surgeon uses tiny instruments to remove blockages-polyps, swollen tissue, or bone that’s narrowing the drainage channels. Success rates? 75-90% of patients report better breathing, less facial pain, and improved smell after FESS. Recovery takes about a week. Most people are back to work in 7-10 days. The key? Surgery doesn’t cure the inflammation. It just opens the doors so medications can work better. For people with nasal polyps, a polypectomy (removal of polyps) is often done at the same time. It gives quick relief-in 85% of cases-but polyps come back in 40-50% of people within 18 months if they don’t keep using steroid sprays afterward.Less Invasive Options: Balloon Sinuplasty
If you’re worried about surgery, there’s another option: balloon sinuplasty. Approved by the FDA in 2005, this procedure uses a tiny balloon catheter. It’s threaded into the blocked sinus, then inflated to gently widen the passageway-like opening a kinked hose. It’s less invasive than FESS. Recovery is faster-most people return to normal in 3-5 days. Studies show 70-80% improvement in drainage and symptoms. But it’s not for everyone. If you have large polyps, severe bone deformities, or extensive scarring, FESS is still the better choice. Balloon sinuplasty works best for people with mild to moderate blockages and no polyps.Biologics: The New Game-Changer
For those with severe chronic sinusitis and nasal polyps who don’t respond to steroids, a breakthrough came in 2019: dupilumab (Dupixent). It’s not a nasal spray. It’s an injection given every two weeks. It targets specific parts of the immune system that drive inflammation. In clinical trials, dupilumab reduced polyp size by 50-60% and improved breathing and smell in 30-40% of patients. It’s now FDA-approved for chronic sinusitis with polyps-and it’s changing lives. One patient in Dublin told me she could smell coffee again for the first time in 10 years after starting it. Other biologics like omalizumab (Xolair) and mepolizumab (Nucala) are also helping. They’re especially useful for people with Samter’s triad-asthma, nasal polyps, and aspirin sensitivity. For these patients, aspirin desensitization (gradually introducing aspirin under medical supervision) improves symptoms in 70-80% of cases. These treatments aren’t cheap, and they’re not first-line. But for those who’ve tried everything else, they’re life-changing.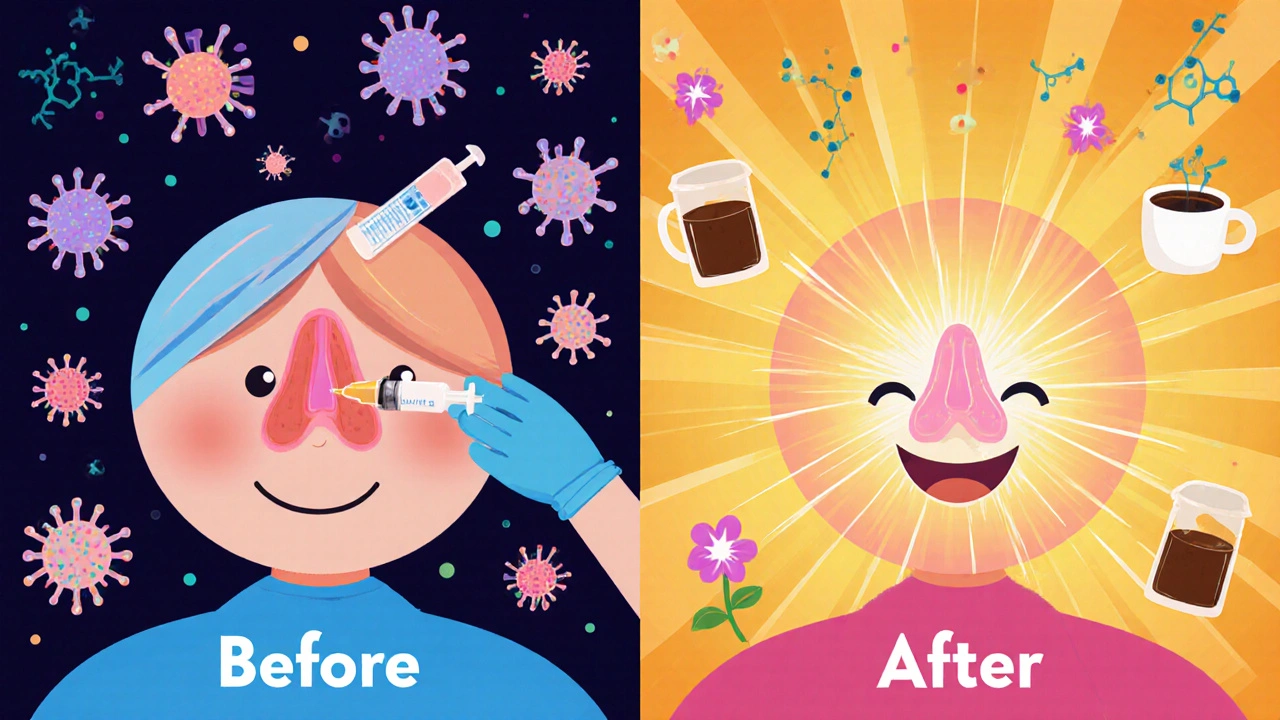
What About Septoplasty?
If you have a deviated septum-a crooked wall between your nostrils-it can block one side of your nose and contribute to chronic sinusitis. About 1 in 5 adults have some degree of deviation. If it’s severe enough to cause blockage, a septoplasty can help. This surgery straightens the septum. It’s often done at the same time as FESS. Studies show 65-75% of patients with both conditions report major improvement after combined surgery. It’s not a cure for inflammation, but it removes a physical barrier so other treatments can work.Long-Term Management Is Key
Chronic sinusitis isn’t something you fix once and forget. It’s a condition you manage. Even after surgery or biologics, you’ll likely need to keep using nasal saline rinses and steroid sprays. Studies show only 55-65% of patients stick with their sprays long-term-often because they don’t feel immediate results. Here’s what actually works for long-term control:- Use a neti pot or squeeze bottle with sterile saline daily.
- Keep your home humidified, especially in winter.
- Avoid smoke, strong cleaners, and known allergens.
- Stay hydrated-thinner mucus drains better.
- See an ENT and allergist together. Coordinated care improves outcomes by 35-45%.
What Happens If You Don’t Treat It?
Most people won’t develop serious complications. But untreated chronic sinusitis can lead to ongoing fatigue, poor sleep, trouble concentrating, and even depression from the constant discomfort. In rare cases-less than 0.5%-infection can spread to the eyes, bones, or brain. That’s why persistent symptoms shouldn’t be ignored. The good news? We know more now than ever about what causes it-and how to treat it. It’s not about more antibiotics. It’s about targeting inflammation, removing blockages, and working with your immune system, not against it.Can chronic sinusitis go away on its own?
No, chronic sinusitis doesn’t typically resolve without treatment. While acute sinusitis clears up in a few weeks, chronic sinusitis lasts 12 weeks or longer and usually requires medical intervention like nasal sprays, rinses, or sometimes surgery. Waiting it out rarely helps and can lead to worsening symptoms or complications.
Is chronic sinusitis caused by bacteria?
In most cases, no. About 70% of chronic sinusitis cases aren’t caused by active bacterial infection. Instead, they’re driven by inflammation from allergies, nasal polyps, or environmental irritants. Antibiotics are rarely effective unless there’s a clear bacterial flare-up.
Do nasal sprays really help?
Yes-when used correctly. Intranasal corticosteroid sprays like Flonase or Nasonex reduce inflammation in 60-70% of patients. But they take 4-8 weeks to work fully. Skipping doses or stopping too soon makes them ineffective. Daily use is key.
What’s the difference between FESS and balloon sinuplasty?
FESS removes tissue and polyps using tiny instruments, while balloon sinuplasty gently widens blocked passages with a balloon. FESS is more effective for severe cases or polyps, with a 75-90% success rate. Balloon sinuplasty has a faster recovery (3-5 days) and works well for mild blockages, but may not last as long.
Are biologics like Dupixent worth considering?
If you have severe chronic sinusitis with nasal polyps and haven’t improved with steroids or surgery, yes. Dupilumab reduces polyp size by half and improves breathing and smell in most patients. It’s not a cure, but it can dramatically improve quality of life when other treatments fail.
Can allergies cause chronic sinusitis even if I don’t sneeze?
Absolutely. You don’t need classic allergy symptoms like sneezing or itchy eyes. Silent allergies can still cause inflammation in your sinuses, leading to congestion, postnasal drip, and loss of smell. If you have asthma or eczema, you’re at higher risk even without obvious hay fever.
Jenny Lee
November 18, 2025 AT 15:24Finally, someone gets it. Nasal sprays aren't magic-they're maintenance. I stopped using mine after two weeks and wondered why nothing changed.
Ram tech
November 20, 2025 AT 09:08lol i thought antibiotics would fix my sinus thing for good. turned out i just paid $300 for a placebo and a sore stomach. #wastedmoney
Evan Brady
November 21, 2025 AT 21:25For real-saline rinses are the unsung heroes here. I used to think they were just for hippies with essential oils. Then I tried it after a brutal winter. My sinuses felt like they'd been let out of jail. Do it daily. No excuses. Your nose will thank you.
mithun mohanta
November 22, 2025 AT 11:41Let’s be honest: FESS isn’t surgery-it’s a spiritual awakening. The moment the endoscope entered, I felt the weight of 12 years of congestion lift… like a phoenix rising from the mucus. My olfactory nerves wept. I smelled rain for the first time since college.
Joshua Casella
November 23, 2025 AT 02:47If you're still relying on antihistamines alone, you're fighting the wrong battle. Allergies are the spark, but inflammation is the wildfire. You need steroids to put out the fire-not just fan the ashes. Coordinated care with an allergist and ENT isn't optional-it's the only path that works.
Richard Couron
November 24, 2025 AT 14:43They don't want you to know this-but biologics are a Big Pharma trap. Dupixent costs $30k/year. Meanwhile, the real cause? 5G towers and fluoride in the water. They're poisoning your sinuses to sell you drugs. You think your polyps are from pollen? Nah. It's the government. Wake up.
Erica Lundy
November 25, 2025 AT 22:07Chronic sinusitis, as described, is less a disease and more a symptom of systemic dysregulation-of immune overactivity, environmental alienation, and the erosion of physiological homeostasis in modern life. The medical paradigm seeks to excise, suppress, or dilate-but rarely to reintegrate. The sinuses, like the gut, are not malfunctioning organs; they are mirrors reflecting the discord between organism and environment. To heal them requires not merely pharmacological intervention, but ecological recalibration: air quality, circadian rhythm, microbial exposure, and psychological stress. Surgery may open the passageways, but only mindfulness can restore the rhythm.
Alex Boozan
November 27, 2025 AT 14:46Anyone who says balloon sinuplasty is ‘less invasive’ is selling you a dream. It’s a temporary band-aid for people too scared to face FESS. The data shows recurrence rates double within 2 years. If you’ve got polyps, you need tissue removal-period. No half-measures. Don’t let fear cost you your sense of smell.
Kevin Jones
November 27, 2025 AT 17:07Biologics are the first true paradigm shift in immunomodulatory ENT since the invention of the nasal corticosteroid. Dupilumab targets IL-4/IL-13-Th2 cytokines that drive type 2 inflammation in CRSwNP. This isn’t symptomatic relief; it’s upstream pathway inhibition. We’re moving from mechanical obstruction management to molecular immunophenotyping. Welcome to precision medicine.