Combination NTI Drugs and Generic Availability: Coverage and Gaps
 Feb, 17 2026
Feb, 17 2026
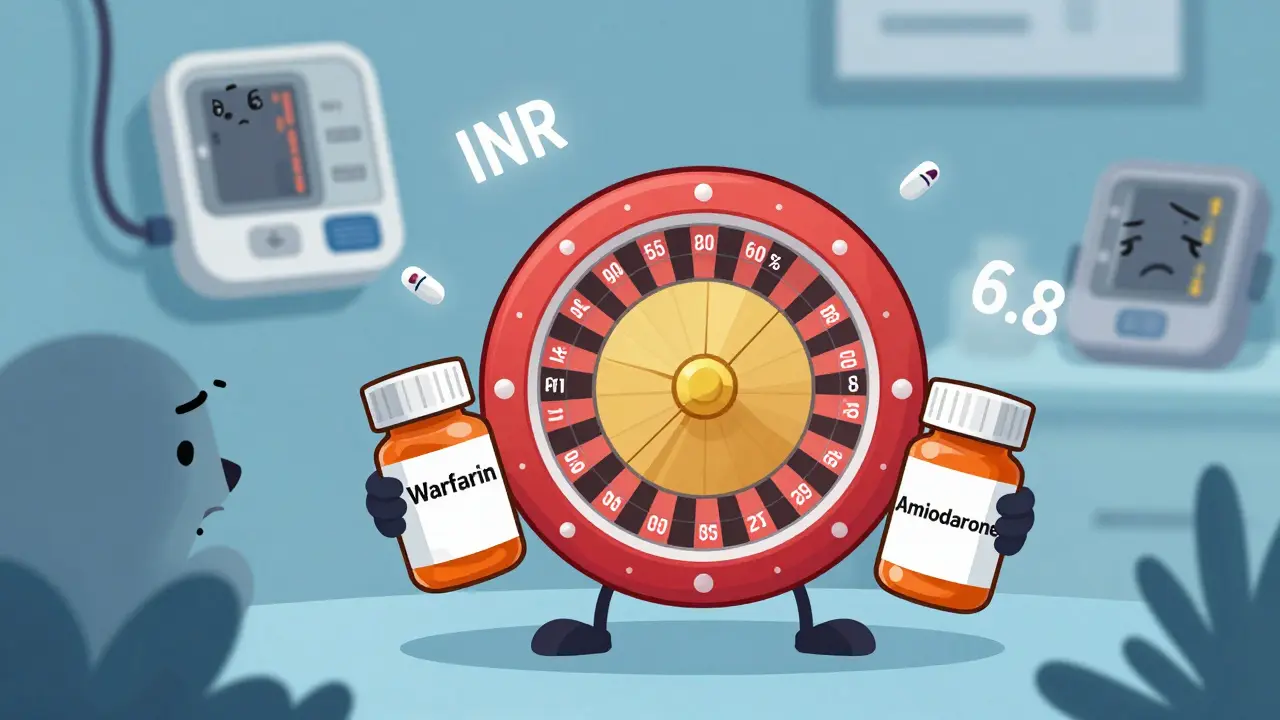
When you take two medications that each have a razor-thin line between working and causing harm, and someone switches one of them to a cheaper generic version, you’re not just changing pills-you’re playing Russian roulette with your health. This is the reality for patients on combination NTI drugs-drugs with a Narrow Therapeutic Index where even tiny changes in blood levels can lead to toxicity or treatment failure. While generics have saved billions in healthcare costs, they’ve created a dangerous blind spot when it comes to combining these high-risk medications. The gap between what’s available and what’s safe is widening, and patients are paying the price.
What Makes a Drug an NTI Drug?
An NTI drug isn’t just any powerful medicine. It’s one where the difference between a therapeutic dose and a toxic dose is so small that a 10% change in blood concentration can mean the difference between recovery and hospitalization. The FDA defines these drugs by five key traits: minimal separation between effective and toxic levels, high risk of life-threatening side effects from small changes, the need for regular blood monitoring, low variation in how your body processes the drug, and frequent small dose adjustments. Think warfarin, lithium, levothyroxine, phenytoin, digoxin. These aren’t optional drugs-they’re often life-savers for heart conditions, thyroid disorders, epilepsy, and psychiatric illnesses.
For single-agent NTI drugs, generic versions exist. About 87% of them do. But when two NTI drugs are combined-say, warfarin and amiodarone for atrial fibrillation-the rules change completely. The margin for error doesn’t just shrink. It vanishes.
Why Combination NTI Drugs Are a Perfect Storm
Imagine two drivers, each with a 10% chance of swerving off the road. If they’re driving separately, you can manage the risk. But if they’re in the same car? Now your chance of crashing is close to 20%. That’s what happens with combination NTI therapy.
Each NTI drug has its own bioequivalence window. For regular drugs, generics must match the brand within 80%-125% of the original’s absorption. For single NTI drugs, that tightens to 90%-111% for peak levels (Cmax) and 90%-112% for total exposure (AUC). But when you combine two NTI drugs? The variations multiply. A 10% difference in one drug plus a 10% difference in the other doesn’t add up to 20%. It compounds. And that’s why the FDA is now proposing even stricter standards-90%-107.69% for Cmax and 90%-110% for AUC for combination NTI products. That’s not just tight. It’s nearly impossible with current manufacturing.
There’s no approved fixed-dose combination of two NTI drugs in the U.S. market. Not one. While generic warfarin is widely available (11 ANDAs approved), no pill exists that combines it with another NTI drug like amiodarone or carbamazepine. Meanwhile, non-NTI combinations-like HIV drugs entecavir and tenofovir-have dozens of generics. The difference? Risk. NTI combinations carry a risk profile that makes regulators and manufacturers nervous. And that nervousness translates into zero options for patients.

The Human Cost of the Gap
Behind every missing generic is a real person. A 2020 JAMA Internal Medicine study found that patients on combination therapies containing even one NTI drug had 27% more adverse events after generic substitution than those on non-NTI combinations. For patients on two NTI drugs? The data isn’t formally tracked-but the anecdotal evidence screams.
A patient on Reddit described switching to generic warfarin and seeing their INR spike from 2.5 to 6.8 in three days. They ended up in the ER. Now imagine both drugs in their regimen were switched. That’s not speculation-it’s the logical outcome. A Drugs.com survey of 1,247 patients on combination NTI therapy found 63.4% had adverse effects after generic substitution. Only 18.2% of those on brand-name combinations reported issues. That’s a threefold difference.
Pharmacists see it too. A 2023 ASHP survey of 856 pharmacists found 78.3% had witnessed therapeutic failure after switching to generics in NTI combinations. Over 40% reported serious events-bleeding, seizures, cardiac arrest. One pharmacist in Ohio told a reporter: "I’ve had patients come in with INRs over 10. They’re not dying from cancer. They’re dying because their pharmacy ran out of the brand-name pill and switched them without a warning."
Why Can’t We Just Make Better Generics?
Manufacturers say they can. Companies like Teva and Sandoz point to Europe, where generic levothyroxine combinations have been used since 2015 with less than 2% adverse events. But here’s the catch: those aren’t true combination NTI drugs. Levothyroxine is NTI, but selenium isn’t. So the combination doesn’t trigger the same risk profile.
The real barrier isn’t technology-it’s science. We don’t have reliable ways to test whether two NTI drugs together behave the same way in the body as the brand-name version. The current bioequivalence studies look at each drug separately. But in a real person, the drugs interact. One might affect how the other is absorbed. Or metabolized. Or cleared. That’s not captured in a lab. Dr. Donald Berry put it bluntly in Nature Reviews Drug Discovery: "The 90-111% window still allows 22% total variation. When you combine two of them, you’re allowing nearly half the system to drift out of safety range."
And the regulatory process? It’s broken. FDA approval for a combination NTI generic takes an average of 4.7 years-more than double the time for non-NTI combinations. Meanwhile, patients wait. Clinicians scramble. Pharmacies have no clear guidance.

What’s Being Done-and What’s Missing
The FDA’s 2023 draft guidance is a step forward. It proposes tighter standards and hints at using pharmacometric modeling-computer simulations of how drugs behave in the body-to predict real-world outcomes. A pilot program is planned for 2024. But it’s still just a draft. No company has submitted an application under these new rules. No product is close to approval.
Meanwhile, patients are stuck. They’re forced to take two separate pills, each potentially generic, with no assurance they’re stable. That’s not a combination. That’s a gamble. And the cost? Patients on combination NTI therapy spend $1,200-$2,500 a year just on therapeutic drug monitoring. That’s triple the cost of non-NTI regimens. And it’s not covered everywhere.
Only 12 of 50 major academic medical centers in the U.S. have specialized clinics for NTI combination therapy. Most community pharmacies don’t have the training. A 2023 ASHP report said pharmacists need over 120 hours of specialized training just to manage these cases. Most don’t have it.
Where Do We Go From Here?
There’s no easy fix. But there are clear steps:
- Stop automatic substitution for any regimen containing an NTI drug. Let prescribers decide, not pharmacists.
- Require explicit labeling on all NTI drugs: "Do not substitute without provider approval."
- Invest in precision testing-use pharmacometric modeling and real-world data to build better bioequivalence standards.
- Expand monitoring access-make therapeutic drug monitoring affordable and widely available.
- Delay generic approval for combination NTI products until science catches up. Better safe than sorry.
Some argue that cost savings justify pushing forward. But when a patient ends up in the ICU because a generic pill was slightly off, the cost isn’t just financial. It’s human. And right now, the system is failing them.
What exactly is an NTI drug?
An NTI (Narrow Therapeutic Index) drug has a very small difference between the dose that works and the dose that causes harm. Even a small change in blood levels can lead to serious side effects or treatment failure. Examples include warfarin, lithium, levothyroxine, phenytoin, and digoxin. The FDA defines these drugs by five key traits: minimal separation between effective and toxic doses, high risk of life-threatening reactions, need for blood monitoring, low variability in how the body processes them, and frequent small dose adjustments.
Why can’t we have generic versions of combination NTI drugs?
Because the bioequivalence standards for combining two NTI drugs are currently impossible to meet with existing manufacturing and testing methods. Each NTI drug already has a very tight acceptable range for absorption (90%-111% for Cmax, 90%-112% for AUC). When you combine two, the total variation can exceed safe limits. The FDA is working on new guidelines, but no company has yet submitted a combination NTI generic for approval. As of 2023, there are zero approved fixed-dose combination NTI products in the U.S.
Are generic NTI drugs safe on their own?
For most patients, yes-when taken as a single agent. About 87% of NTI drugs have generic versions, and many work well. But studies show that even with single NTI drugs, about 18.7% of patients on generic warfarin experience unstable INR levels compared to 4.3% on brand-name. So while generics aren’t universally unsafe, they require close monitoring and aren’t risk-free.
What are the risks of switching to generic in a combination NTI regimen?
The risks are severe. A 2020 study found 27% more adverse events in patients on combination therapies with one NTI drug after generic substitution. For two NTI drugs, the risk multiplies. Patients have reported life-threatening INR spikes, seizures, and cardiac events. A Drugs.com survey showed 63.4% of patients on combination NTI drugs had adverse effects after switching to generics-compared to 18.2% on brand-name. The combination effect isn’t just additive-it’s exponential.
What should patients do if they’re on combination NTI drugs?
Ask your prescriber if your medications are NTI drugs. If they are, insist on staying on the brand-name version if possible. Never accept a generic substitution without explicit approval from your doctor. Monitor symptoms closely-especially if you’re on warfarin, lithium, or similar drugs. Keep a log of side effects and share it with your pharmacist. If your pharmacy switches your meds without asking, speak up. You have the right to refuse substitution.
Is there any progress being made to fix this issue?
Yes. The FDA released draft guidance in February 2023 proposing even tighter bioequivalence standards for combination NTI drugs: 90%-107.69% for Cmax and 90%-110% for AUC. They’re also planning a 2024 pilot using computer modeling to predict how these drugs behave together. But these are still in development. No product is close to approval, and it could take years before any combination NTI generic reaches the market.