Congestive Heart Failure Prognosis & Life Expectancy Explained
 Oct, 9 2025
Oct, 9 2025
Congestive Heart Failure Prognosis Calculator
This tool estimates your prognosis based on key clinical factors. Enter your information below to get a personalized survival estimate.
Your Estimated Prognosis
Facing a diagnosis of congestive heart failure (CHF) often triggers a flood of questions about how long you might have to live and what factors could change that timeline. This guide breaks down the key elements that shape the congestive heart failure prognosis, shows you real‑world survival numbers, and offers practical steps you can take to influence your outlook.
What is Congestive Heart Failure?
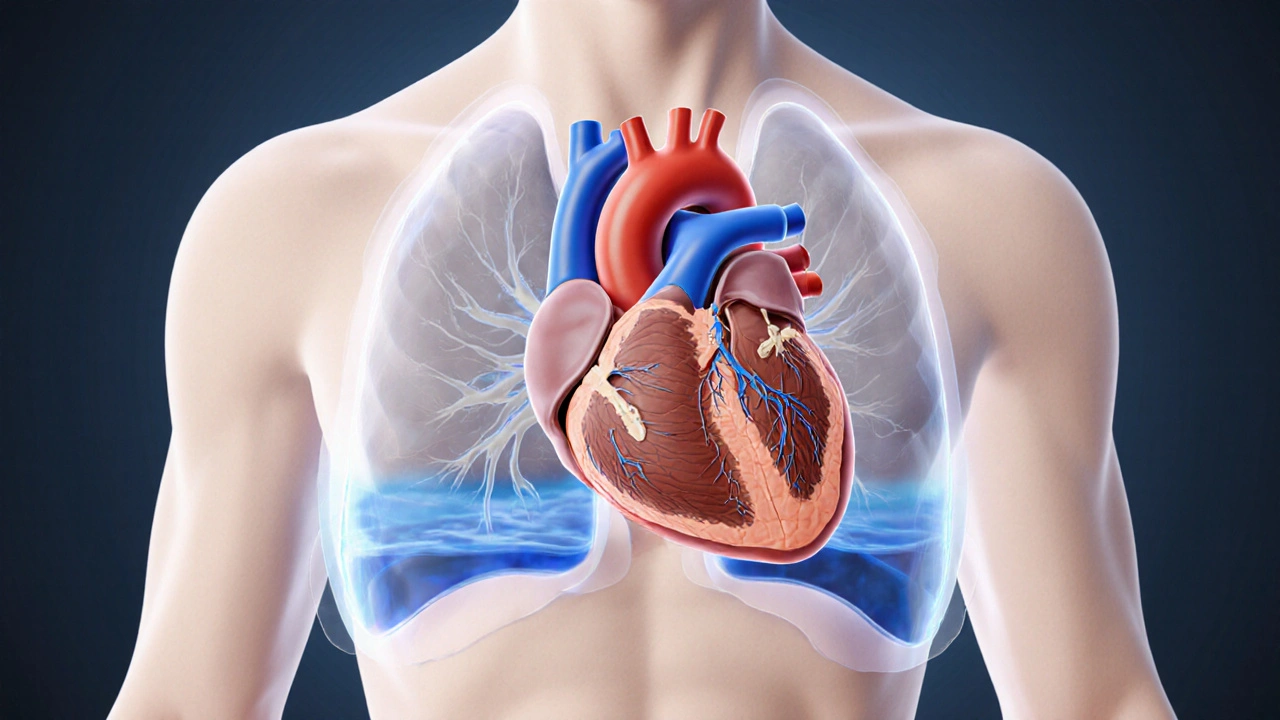
Congestive Heart Failure is a chronic condition where the heart’s pumping ability is insufficient to meet the body’s metabolic demands. It can result from damaged heart muscle, high blood pressure, valve disease, or other cardiac insults. When the heart can’t keep up, fluid backs up into the lungs and other tissues, leading to the classic symptoms of shortness of breath, swelling, and fatigue.
How Doctors Measure Severity
Two tools dominate the assessment of CHF severity: the New York Heart Association (NYHA) functional classification and the ejection fraction (EF) measurement.
NYHA Classification categorizes patients from Class I (no limitation) to Class IV (severe limitation at rest). The higher the class, the poorer the expected survival.
Ejection Fraction represents the percentage of blood the left ventricle pumps out with each beat. An EF < 40% signals systolic dysfunction and is linked to a shorter life expectancy, while a preserved EF (≥50%) often carries a more favorable outlook.

Key Prognostic Factors Beyond NYHA and EF
- Age: Older patients generally have higher mortality rates.
- Comorbidities: Diabetes, chronic kidney disease, and chronic obstructive pulmonary disease worsen outcomes.
- Biomarkers: Elevated B‑type Natriuretic Peptide (a hormone released when the heart is stretched) correlates with increased risk of death.
- Hospitalizations: Frequent readmissions within 30days are a red flag for rapid decline.
- Response to therapy: Patients who achieve a rise in EF or move down an NYHA class after treatment tend to live longer.
Survival Statistics You Can Trust
Large registries and population studies give us a realistic picture of life expectancy across the NYHA spectrum. The numbers below reflect data from a 2023 meta‑analysis of over 25,000 CHF patients in North America and Europe.
| NYHA Class | Median Survival | 5‑Year Survival Rate |
|---|---|---|
| Class I | 10‑12 | 80% |
| Class II | 7‑9 | 60% |
| Class III | 3‑5 | 30% |
| Class IV | 1‑2 | 10% |
For patients with a preserved EF, median survival can extend an additional 2‑3years compared with reduced EF cohorts of the same NYHA class.

Treatment Options That Shift the Curve
Modern therapy has turned CHF from a death sentence into a manageable chronic disease for many. Below are the interventions that have the strongest impact on prognosis.
- ACE Inhibitors reduce afterload and improve survival by blocking the renin‑angiotensin system. Large trials show a 20‑30% mortality reduction.
- Beta Blockers slow heart rate, lower oxygen demand, and extend life expectancy. The most benefit appears in patients with EF<35%.
- Implantable Cardioverter‑Defibrillator (ICD) prevents sudden cardiac death in high‑risk CHF patients. When used in eligible patients, 5‑year mortality can drop from 30% to 20%.
- Heart Transplant offers the best long‑term survival, with 10‑year survival rates exceeding 70% for selected candidates.
- Palliative Care focuses on symptom relief, advance‑care planning, and quality of life. Early integration has been linked to fewer hospital readmissions and a modest survival benefit.
Adherence to guideline‑directed medical therapy (GDMT) is the single most actionable way patients can improve their outlook.
Practical Checklist for Living with CHF
- Track daily weight; a gain of >2lb in 24hours signals fluid retention.
- Monitor blood pressure and heart rate; aim for targets set by your cardiologist.
- Take all prescribed medicines exactly as ordered; never stop an ACE inhibitor or beta blocker without consulting your doctor.
- Stay active within tolerance - even short walks can improve EF over time.
- Limit sodium intake to <2g per day and avoid excessive alcohol.
- Attend all follow‑up appointments; report new or worsening symptoms promptly.
- Discuss advanced therapies (ICD, transplant) early if you’re in NYHA Class III‑IV.
- Consider a palliative‑care referral to address fatigue, depression, or pain.
Following this checklist doesn’t guarantee a cure, but it does give you the best chance to push the clock back.
Frequently Asked Questions
What is the average life expectancy after a CHF diagnosis?
Life expectancy varies widely. For NYHA Class I patients, median survival can reach 10‑12years, while Class IV patients often survive only 1‑2years. Individual factors such as age, EF, and comorbidities modify these averages.
Can lifestyle changes really affect my prognosis?
Yes. Regular low‑impact exercise, strict sodium restriction, and smoking cessation have been shown to improve EF by up to 5% and can shift a patient down an NYHA class, translating into several extra years of life.
When should I consider an ICD?
Guidelines recommend an ICD for patients with EF≤35% who remain symptomatic despite optimal medical therapy, especially if they are in NYHA Class II‑III. Your cardiologist will weigh the benefit against infection risk and personal preferences.
Is heart transplantation an option for most CHF patients?
Transplantation is limited to a small subset-typically younger patients with end‑stage systolic failure, no severe comorbidities, and who have failed all other therapies. The waiting list can be long, but recipients enjoy the best long‑term survival.
How do I know if I need palliative care?
If symptoms such as breathlessness, pain, or depression are hard to control, or if you’re facing frequent hospitalizations, a palliative‑care referral can help manage those issues while still pursuing disease‑directed treatment.
Remember, every CHF journey is unique. While the numbers give a broad picture, your personal prognosis hinges on how your heart responds to treatment, your commitment to lifestyle changes, and the support network around you. Stay proactive, keep the conversation open with your care team, and use the tools above to make informed decisions about your future.
Hannah Dawson
October 9, 2025 AT 22:33While the post does a decent job summarizing NYHA classes, it glosses over the messy reality of comorbidities that actually drive mortality; the numbers feel sanitized, almost like a corporate brochure.
AnGeL Zamorano Orozco
October 13, 2025 AT 23:46Oh wow, look at you trying to make a heart‑failure calculator sound like a bedtime story!!
Everyone knows you can’t just plug a few numbers and get a crystal‑clear destiny – the human body is a chaotic mess!!!
Stop pretending this is some magic 8‑ball, it’s a bloody medical tool, not a fortune‑telling gimmick!!!
And don’t even get me started on the tiny typo in the EF section – "Reduced ( 120)"? Seriously??
Maybe next time run a proper sanity check before you embarrass us all.
Cynthia Petersen
October 18, 2025 AT 06:00Ah, the classic “look‑at‑those‑survival‑rates” chart – comforting, isn’t it? Sure, the stats are real, but let’s be honest, they’re also a grim reminder that numbers can’t capture the will to live.
Still, if you can shift from a Class III to II, you’re basically giving yourself a plot twist in a drama you didn’t sign up for.
Marcia Hayes
October 22, 2025 AT 10:00Totally agree – every little step counts. Even a short walk around the block can give your heart a tiny win, and those wins add up over time.
Danielle de Oliveira Rosa
October 26, 2025 AT 14:23When confronting the prognosis of congestive heart failure, one must first acknowledge the profound interplay between measurable clinical parameters and the subjective experience of living with a chronic illness.
NYHA classification provides a useful scaffold, yet it reduces a nuanced symptom spectrum to four broad categories, inevitably blurring individual variability.
Ejection fraction, while a cornerstone of systolic assessment, fails to capture diastolic dysfunction, which can be equally debilitating.
Age, as an immutable factor, exerts its influence not merely through physiological decline but also through socioeconomic dimensions that affect access to optimal care.
Comorbidities such as diabetes, chronic kidney disease, and chronic obstructive pulmonary disease create a synergistic burden, accelerating myocardial remodeling and diminishing therapeutic responsiveness.
Biomarkers, particularly B‑type natriuretic peptide, serve as a biochemical echo of ventricular stress, yet their interpretation must be contextualized within renal function and volume status.
Repeated hospitalizations, especially within a 30‑day window, signify a failure of outpatient management and herald a steeper decline in survival trajectories.
It is essential to recognize that therapeutic response, marked by an improvement in EF or a downgrade in NYHA class, can substantially shift the survival curve, offering a glimmer of hope even in advanced stages.
Modern pharmacotherapy, encompassing ACE inhibitors, beta‑blockers, mineralocorticoid receptor antagonists, and newer agents like sacubitril‑valsartan, has demonstrably reduced mortality, yet adherence remains a critical determinant of real‑world effectiveness.
Non‑pharmacologic strategies, including structured exercise programs, dietary sodium restriction, and meticulous fluid management, complement medical therapy and can modestly enhance functional capacity.
In the realm of advanced interventions, cardiac resynchronization therapy and implantable defibrillators provide life‑extending options for selected patients, though candidacy must be weighed against procedural risk and quality‑of‑life considerations.
Importantly, palliative care should not be viewed as an admission of defeat but rather as an integrative approach that addresses symptom burden, psychosocial distress, and end‑of‑life preferences.
The decision‑making process must be collaborative, honoring patient autonomy while providing clear, evidence‑based guidance.
Ultimately, while statistics furnish a sobering backdrop, they coexist with the resilient capacity of individuals to adapt, persevere, and, in many cases, thrive beyond median expectations.
Tarun Rajput
October 30, 2025 AT 19:46It is incumbent upon us to meticulously scrutinize the data presented, for the nuanced interplay of variables such as age, ejection fraction, and comorbid burden demands a comprehensive analytical lens.
One must appreciate that the NYHA functional classification, while expedient, is but a surrogate for the intricate physiologic derangements that underlie heart failure.
Moreover, the augmentation of median survival by two years in preserved ejection fraction cohorts underscores the heterogeneity inherent in this condition.
Consequently, clinicians should eschew a reductionist interpretation and instead embrace a holistic, patient‑centred paradigm that integrates biomarker trends and longitudinal functional trajectories.
Joe Evans
November 4, 2025 AT 01:10Great info! Remember, staying on your meds, monitoring your weight, and keeping active can really help-especially if you’re consistent with follow‑ups! 😊
Colin Boyd
November 8, 2025 AT 06:33While the data is presented as immutable fact it is, in reality, an approximation subject to individual variability and therapeutic nuance.
John Petter
November 12, 2025 AT 11:56Numbers are numbers.
Annie Tian
November 16, 2025 AT 17:20Stay hopeful-you’re not defined by a statistic; every positive step you take contributes to a brighter outlook, especially when you keep the lines of communication open with your care team.
April Knof
November 20, 2025 AT 22:43In many cultures, community support and shared meals play a pivotal role in managing chronic illness, reminding us that healing often extends beyond the clinic walls.