Estriol Cream vs Alternatives: Which Estrogen Treatment is Right for You?
 Oct, 14 2025
Oct, 14 2025
Key Takeaways
- Estriol cream offers milder estrogenic activity, making it a popular choice for mild vaginal atrophy and skin dryness.
- Estradiol creams provide stronger potency and faster symptom relief but may carry higher risk of systemic side effects.
- Non‑prescription moisturizers and phytoestrogen gels work for surface dryness but lack the deep tissue benefits of true estrogen creams.
- Cost, availability, and personal health history are the biggest factors when deciding between options.
- Always discuss with a healthcare professional before starting any estrogen‑based product.
Many women navigating menopause wonder whether estriol cream is the best fit for their skin and vaginal health or if other estrogen products or even non‑hormonal moisturizers would work better. Below we break down the most common alternatives, compare their key attributes, and give you a clear checklist to decide which route aligns with your needs.
Estriol Cream is a low‑potency estrogen formulated for topical use on the vagina or vulvar area. Its primary function is to replenish estrogen levels locally, easing dryness, itching, and mild atrophic changes without causing significant systemic absorption. First introduced in the 1990s, estriol (E3) is one of the three natural human estrogens, known for being the weakest but also the safest when applied locally.
To help you compare, we’ll look at four major alternatives:
- Estradiol Cream - a stronger, prescription‑only estrogen (E2) used for similar vaginal and skin symptoms.
- Conjugated Estrogen Cream - a blend of estrogen types derived from horse urine, sold under brand names like Premarin.
- Phytoestrogen Cream - a plant‑based, over‑the‑counter moisturizer containing soy or red clover extracts.
- Standard Moisturizing Cream - non‑hormonal emollients such as hyaluronic acid or glycerin based products.
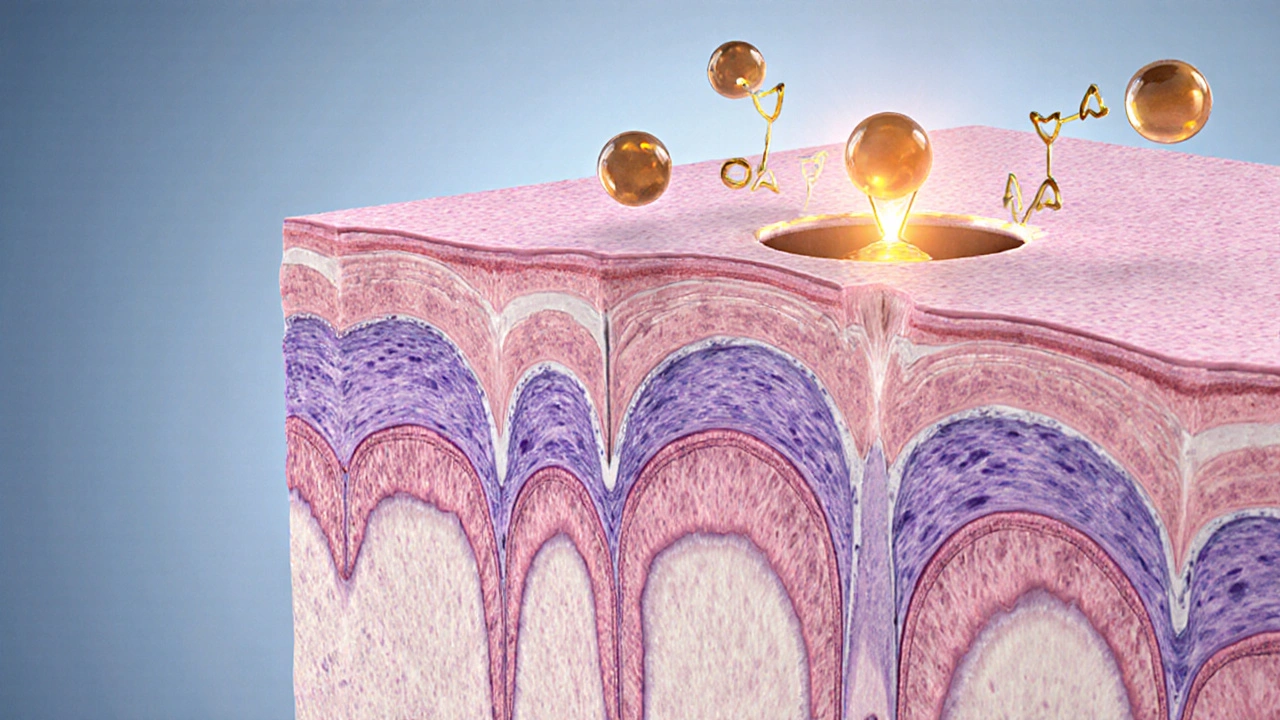
How Estriol Cream Works
Estriol binds to estrogen receptors (ERα and ERβ) but activates them less vigorously than estradiol. This lower activation translates into:
- Reduced risk of stimulating estrogen‑sensitive tissues like the breast and uterus.
- Less impact on blood clotting factors, making it a safer option for women with a history of thrombosis.
- Gradual improvement of the vaginal epithelium, restoring elasticity and moisture over weeks rather than days.
Because the systemic absorption is minimal-studies show serum estriol levels increase by less than 10% after daily use-the cream is often recommended for women who want symptom relief without the systemic commitment of oral hormone replacement therapy (Hormone Replacement Therapy).
Alternative #1: Estradiol Cream
Estradiol Cream contains the more potent estrogen E2, the same hormone that dominates the pre‑menopausal cycle. Typical concentrations range from 0.01% to 0.1% (0.1mg/g to 1mg/g). Because it’s stronger, users often notice:
- Quicker relief-often within 3‑5 days-of vaginal dryness and burning.
- Greater improvement in urinary urgency for women with mild incontinence.
- A slightly higher chance of systemic side effects such as breast tenderness or spotting.
Estradiol cream is a prescription product in the US, UK, and most EU countries, meaning a doctor must assess your risk profile before prescribing.
Alternative #2: Conjugated Estrogen Cream (Premarin)
Conjugated estrogen blends several estrogen molecules (mainly estrone sulfate and equine estriol). It’s been used for decades to treat menopausal symptoms. As a cream, it’s typically available in 0.5mg/g or 1mg/g strengths. Benefits include:
- Broad spectrum of estrogen activity, useful for women who didn’t respond well to single‑molecule formulations.
- Established safety data from large clinical trials.
The downside is a higher overall estrogen load, which may increase the risk of endometrial hyperplasia if used without a progestogen in women with a uterus.
Alternative #3: Phytoestrogen Cream
Phytoestrogens are plant‑derived compounds that weakly bind to estrogen receptors. Common sources are soy isoflavones and red clover. These creams are sold OTC and marketed as “natural” alternatives. They work by:
- Providing a gentle estrogenic signal that can modestly improve superficial skin hydration.
- Often containing additional moisturizers like shea butter for barrier repair.
Because the estrogenic effect is mild, most users see only subtle improvements in dryness and no measurable change in vaginal epithelium thickness.
Alternative #4: Standard Moisturizing Cream
Non‑hormonal moisturizers (e.g., hyaluronic acid gels, glycerin‑based ointments) focus purely on surface hydration. They are safe for all women, including those with estrogen‑sensitive cancers, but they do not address the underlying estrogen deficiency that causes atrophic changes.
Typical outcomes include short‑term relief of itching and burning, but the benefits disappear quickly once you stop applying the product.
Side‑by‑Side Comparison
| Product | Typical Concentration | FDA / EMA Status | Primary Use | Onset of Relief | Common Side Effects | Cost (USD per month) |
|---|---|---|---|---|---|---|
| Estriol Cream | 0.01% - 0.03% (0.1mg/g - 0.3mg/g) | Prescription (US/EU) | Vaginal atrophy, mild skin dryness | 1‑2weeks | Minor burning, rare spotting | $30‑$70 |
| Estradiol Cream | 0.01% - 0.1% (0.1mg/g - 1mg/g) | Prescription (US/EU) | Vaginal atrophy, urinary symptoms | 3‑5days | Breast tenderness, spotting | $45‑$120 |
| Conjugated Estrogen Cream | 0.5mg/g - 1mg/g | Prescription (US/EU) | Broad menopausal relief | 1‑2weeks | Endometrial thickening, nausea | $55‑$130 |
| Phytoestrogen Cream | Varies (usually <1mg/g of isoflavones) | OTC (US/EU) | Surface hydration, mild estrogenic support | 2‑4weeks | None significant | $20‑$50 |
| Standard Moisturizing Cream | Not applicable | OTC (US/EU) | Barrier repair, short‑term relief | Immediate | Rare irritation | $10‑$30 |
Decision Checklist - Which Option Fits You?
- Do you need rapid symptom relief? If yes, estradiol cream’s faster onset may be worth the slightly higher side‑effect profile.
- Are you concerned about systemic estrogen exposure? Estriol cream’s low absorption makes it the safest hormonal choice.
- Do you have a uterus and cannot take progestogen? Avoid conjugated estrogen cream unless paired with a progesterone regimen.
- Is cost a major factor? Over‑the‑counter phytoestrogen or standard moisturizers are the cheapest, but they won’t correct tissue thinning.
- Do you have a history of estrogen‑sensitive cancer? Stick with non‑hormonal moisturizers or discuss a very low‑dose estriol regimen with your oncologist.
Practical Tips for Using Estriol Cream Effectively
Even the right product can fall short if you don’t apply it correctly. Follow these steps:
- Wash hands and the applicated area with mild, fragrance‑free soap. \n
- Pat the skin dry-don’t rub, as this can irritate delicate tissue.
- Apply a pea‑size amount (about 0.5g) to the targeted area. Use a clean fingertip or the supplied applicator.
- Massage gently for 30seconds to help absorption.
- Wait at least 30minutes before inserting tampons, douching, or having intercourse.
- Store the tube at room temperature, away from direct sunlight.
Most clinicians recommend once‑daily use for the first two weeks, then taper to 2‑3 times per week for maintenance.
When to Seek Professional Advice
If you notice any of the following, contact your healthcare provider promptly:
- Persistent vaginal bleeding or spotting after more than two weeks of use.
- Sudden breast tenderness, lumps, or discharge.
- Severe burning or allergic reaction at the application site.
- New onset pelvic pain or urinary retention.
These symptoms could signal systemic absorption or an unrelated condition requiring further evaluation.
Future Trends in Topical Estrogen Therapy
Research is moving toward ultra‑low‑dose formulations that release estriol over 24hours, aiming to further minimize systemic exposure. Additionally, microneedle patches are being explored to deliver estrogen directly into the dermis, offering precise dosing without mess.
As personalized medicine evolves, genetic testing may soon help clinicians predict which women will respond best to estriol versus estradiol, making the choice less guess‑work and more data‑driven.
Frequently Asked Questions
Can I use estriol cream if I have a history of breast cancer?
Estriol’s weak estrogenic activity makes it one of the safer hormonal options for women with a remote or low‑risk breast cancer history, but you must get clearance from your oncologist. Some specialists still prefer non‑hormonal moisturizers to eliminate any estrogen exposure.
How long does it take to see tissue changes with estriol cream?
Clinical studies show measurable improvement in vaginal epithelial thickness after about 2-3weeks of daily use, with peak benefits often reached at 8weeks.
Is it safe to use estriol cream together with a condom?
Yes. Because estriol cream is applied locally and absorbs minimally, it does not degrade latex. However, wait at least 30minutes after application to avoid reducing condom effectiveness.
Can I switch from estradiol cream to estriol cream without a wash‑out period?
Most clinicians advise a short overlap of 2‑3days or a brief pause to monitor any lingering systemic estrogen levels, especially if you’ve been on a high‑dose estradiol regimen.
Do phytoestrogen creams work for severe vaginal atrophy?
They may improve surface moisture but lack the potency to reverse significant atrophic thinning. For moderate to severe cases, a prescription estrogen cream like estriol or estradiol is usually required.
Hariom Godhani
October 14, 2025 AT 18:35It is baffling how many women still wander the pharmacy aisles, clutching cheap moisturizers, believing they can substitute genuine estrogen therapy with a scented lotion. The truth, my dear readers, is that estriol cream is not a gimmick; it is a meticulously engineered low‑potency estrogen that has been scientifically validated to rebuild the vaginal epithelium with minimal systemic spillover. While the market showers you with a cacophony of “natural” alternatives, most of them are nothing more than glorified butter creams that lack any credible receptor activity. You cannot expect a soy‑infused bottle to thicken vaginal walls when the very molecules barely whisper to ERβ. Moreover, the notion that a cheaper over‑the‑counter product will spare you from the modest risk of endometrial hyperplasia is a dangerous myth that endangers both health and dignity. Let us be clear: the modest increase in serum estriol after topical application is precisely why it is tolerated by women with a history of thrombosis; it does not translate into the systemic estrogen surge that fuels breast tissue proliferation. If you are terrified of the specter of breast tenderness, the low‑dose nature of estriol makes it the logical first line, not a desperate last‑ditch effort after failed estradiol regimens. Conversely, prescribing estradiol cream without assessing personal risk factors can be tantamount to playing roulette with your cardiovascular profile. The table of side‑effects in the article underscores a stark reality: stronger does not always mean better, especially when the patient’s uterus or breast is already susceptible. Physicians who dismiss estriol as “too weak” are failing their patients by ignoring the principle of “the lowest effective dose.” In the hierarchy of estrogenic preparations, estriol occupies a niche that balances efficacy with safety, a balance that many “natural” products simply cannot achieve. Remember, the price tag of $30‑$70 per month reflects not only the active ingredient but also rigorous compounding standards that unregulated moisturizers lack. Do not be seduced by the allure of “plant‑based” creams that claim to be “hormone‑free” while delivering negligible clinical benefit. Ultimately, the decision rests on a personalized risk‑benefit analysis, but let the data speak louder than marketing hype. Choose estriol when you desire steady, modest improvement without courting systemic complications. Reject the myth that “all creams are the same” and demand evidence‑based therapy that respects your body’s delicate hormonal equilibrium.
Jackie Berry
October 22, 2025 AT 00:35I totally get the confusion that springs up when you stare at the endless list of estrogen options – it can feel like a maze with no clear exit. Estriol cream, with its gentle touch, often serves as a comfortable starting point for many women dealing with mild dryness. If you’ve got a history of blood clots, the lower systemic absorption can be a real peace of mind. On the other hand, if you’re battling more severe symptoms, the quicker kick‑in of estradiol might be what you need. It’s also worth noting that non‑prescription moisturizers can be a nice adjunct, but they don’t replace the deeper tissue benefits that true estrogen provides. Talk with your healthcare provider about your personal health story; they can help you weigh the pros and cons in a way that feels right for you.
Bottom line: there’s no one‑size‑fits‑all, and finding the right fit is a journey worth taking.
Mikayla May
October 29, 2025 AT 05:35For anyone looking for a quick rundown: estriol cream offers mild estrogenic activity with minimal systemic effects, making it a safe option for most women. Estradiol cream works faster and stronger but can cause breast tenderness or spotting. Conjugated estrogen has broader estrogen activity and may need a progestogen if you have a uterus. Phytoestrogen creams are gentle but only improve surface hydration. Regular moisturizers hydrate the outer layer but won’t reverse atrophy. Always check with your doctor before starting.
Jimmy the Exploder
November 5, 2025 AT 11:35These creams are just marketing hype
Robert Jackson
November 12, 2025 AT 17:35It is incumbent upon the discerning reader to recognize that the pharmacokinetic profile of estriol is fundamentally distinct from that of estradiol, rendering any attempt to equate the two as scientifically untenable. The assertion that “all estrogen creams work the same” not only betrays a superficial understanding of receptor affinity but also disregards the extensive peer‑reviewed literature delineating estriol’s reduced affinity for ERα relative to ERβ. Consequently, the systemic exposure risk is markedly attenuated, a fact corroborated by multiple randomized controlled trials. Moreover, the therapeutic index of estriol, when applied topically, situates it as the optimal compromise between efficacy and safety for the majority of post‑menopausal patients. To neglect these nuances in clinical decision‑making would constitute a dereliction of professional duty.
Robert Hunter
November 19, 2025 AT 23:35From a global perspective, the availability of estriol cream varies widely, yet its benefits remain universally relevant. Many women in regions with limited access to prescription hormones still manage symptoms with locally sourced plant‑based gels, but these lack the proven receptor activation that estriol delivers. If you can obtain a compounding pharmacy that offers a standardized estriol formulation, you are likely to see measurable improvement in vaginal moisture and elasticity. I encourage you to explore reputable sources and discuss with a clinician who understands both the cultural context and the pharmacology.
Shruti Agrawal
November 27, 2025 AT 05:35It sounds like you’re feeling overwhelmed by all the choices It can be hard to decide which product will work best for you but remember that estriol is known for its gentle action and low risk if you have a clotting history you might feel more comfortable with it while estradiol works faster but may cause more side effects a simple moisturizer can help with surface dryness but won’t fix deeper issues talk to your doctor and they can help you pick the right option
Katey Nelson
December 4, 2025 AT 11:35Isn’t it fascinating how the pursuit of comfort in our intimate spaces mirrors the larger quest for balance in life? 😏 When we choose a cream, we’re not just selecting a product; we’re negotiating with our own bodies, the expectations of society, and the whispers of the pharmaceutical industry. Estriol, with its subtle estrogenic whisper, seems to say “I’m here, but I won’t dominate” while estradiol shouts “I’ll fix you now!” and the phyto‑remedies murmur “nature knows best.” The irony is that the most “natural” options often lack the scientific backing that makes a real difference, leaving us trapped in a cycle of trial, error, and disappointment. 🍃 Yet, the safety profile of estriol can bring a sense of calm to those wary of systemic effects, especially if you’ve walked the tightrope of thrombosis risk. Ultimately, the decision reflects a deeper philosophical stance: do we prefer gentle consistency or bold immediacy? Choose wisely, dear reader, for your body deserves both love and logic. 😊
Joery van Druten
December 11, 2025 AT 17:35When evaluating options, consider the following checklist: 1) Desired speed of symptom relief – estradiol typically provides faster improvement. 2) Risk tolerance – estriol has lower systemic absorption, suitable for clotting concerns. 3) Cost – over‑the‑counter moisturizers are cheapest but lack tissue regeneration. 4) Prescription requirement – both estriol and estradiol need a prescription in most countries. 5) Personal health history – uterus, breast cancer risk, and cardiovascular profile should guide therapy. Use this framework to have a focused conversation with your clinician.
Melissa Luisman
December 18, 2025 AT 23:35Stop believing that “any cream will do” – the data is crystal clear. Estriol’s low potency means it won’t flood your system with estrogen, which is exactly why it’s safe for women with clotting histories. Estradiol, on the other hand, delivers rapid symptom relief but brings a higher chance of breast tenderness and spotting. Phytoestrogen creams are essentially placebos for deeper atrophy. If you want real, lasting improvement, you need a prescription‑grade estrogen cream, not a grocery‑store moisturizer.
Akhil Khanna
December 26, 2025 AT 05:35Hey everyone 😊 I just wanted to add that the choice isn’t just about the cream it’s also about how comfortable you feel with your body and the healthcare system 💪 Estriol is a great starter if you’re worried about clotting risk – it’s gentle yet effective 🌸 If you need faster relief and your doc says it’s safe, estradiol can be a good next step 🔬 Remember, non‑prescription moisturizers can help with surface dryness but won’t fix deeper tissue changes – so use them as a supplement not a replaceement. Stay positive and keep asking questions! 🙏
Zac James
January 2, 2026 AT 11:35Across different healthcare systems, the accessibility of estriol versus estradiol varies, but the underlying pharmacology remains consistent. Patients who prioritize minimal systemic exposure often opt for estriol, while those seeking quicker symptom control may prefer estradiol despite its higher side‑effect profile. It’s useful to compare cost, insurance coverage, and individual health history when making a decision.
Arthur Verdier
January 9, 2026 AT 17:35Oh sure, because the big pharma gentlemen in white coats are totally out to help us find the “perfect” cream, right? 🙄 They’ve hidden the secret that estriol is actually a mind‑control serum, but we’ll ignore that because we all love a good placebo. In reality, the “natural” phyto‑creams are just a way for them to keep us buying more products while they skim the profits. If you really want to avoid the Illuminati’s estrogen agenda, stick to plain water and call it a day.
Breanna Mitchell
January 16, 2026 AT 23:35It’s wonderful to see how many options are out there – that means there’s something for everyone! Remember, the best choice is the one that aligns with your health goals and comfort level. If estriol feels right for you, give it a try and monitor how you feel. You’ve got this, and your body will thank you for the thoughtful care you’re giving it.
Alice Witland
January 24, 2026 AT 05:35Well, isn’t it just delightful that we have yet another spreadsheet of estrogen creams to parse? One could almost feel the excitement of reading tables while the real issue – personal comfort – gets sidelined. Nonetheless, if you’re after a low‑risk option, estriol does appear less likely to cause systemic woes. Conversely, if you need rapid relief and can tolerate a bit of spotting, estradiol is the obvious candidate. In any case, a brief chat with your GP should settle the matter without too much drama.
Andy V
January 31, 2026 AT 11:35Let me point out the numerous grammatical inconsistencies scattered throughout the article: “low‑potency estrogen formulated for topical use on the vagina or vulvar area” should read “low‑potency estrogen formulated for topical use on the vaginal or vulvar area.” Additionally, “the cream is often recommended for women who want symptom relief without the systemic commitment of oral hormone replacement therapy” would be clearer as “the cream is often recommended for women who want symptom relief without the systemic commitment of oral hormone‑replacement therapy.” Such errors, though minor, undermine the credibility of the piece.
Tammie Sinnott
February 7, 2026 AT 17:35Picture this: a woman standing at the crossroads of comfort and risk, clutching a tube of estriol cream in one hand and a prescription for estradiol in the other. The drama unfolds as she weighs the gentle whisper of estriol against the thunderous roar of estradiol’s rapid relief. In the end, the decision hinges on her personal health narrative – a history of thrombosis calls for caution, while severe atrophy may demand potency. Both pathways have their champions, and both demand respect. Choose wisely, for the story of your body is still being written.