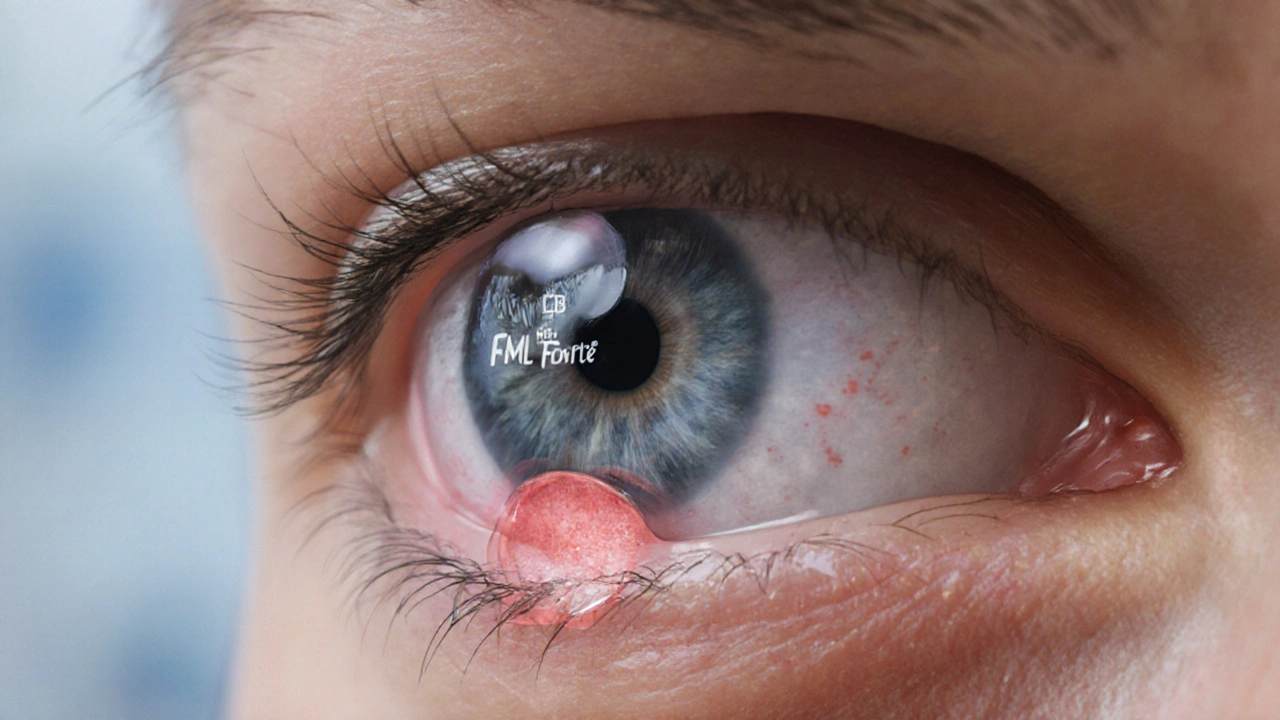
FML Forte (Fluorometholone) vs Alternatives: Quick Comparison for Eye Inflammation
 Sep, 27 2025
Sep, 27 2025
Ophthalmic Drop Comparison Tool
Select Your Conditions and Preferences
Based on your needs, we'll recommend the best ophthalmic drop for your eye inflammation.
FML Forte is a topical ophthalmic corticosteroid containing 0.1 % fluorometholone, used to calm inflammation after surgery or injury. It belongs to the fluorinated steroid class and is prized for its low intra‑ocular pressure (IOP)‑raising potential compared with older steroids.
When your eye feels gritty, red, and painful, the instinct is to reach for a drop that promises fast relief. The challenge is picking a formulation that eases the swelling without sowing the seeds for cataract formation or pressure spikes. This guide walks you through the most prescribed alternatives, highlights what sets them apart, and gives you a simple decision matrix to choose the safest, most effective option for your situation.
How Fluorometholone Works
Fluorometholone is a medium‑potency glucocorticoid that binds to intracellular receptors, switching off inflammatory genes and stabilising cell membranes. Its fluorine atom improves lipid solubility, allowing better corneal penetration while reducing mineralocorticoid activity - the reason it tends to keep IOP lower than classic steroids such as dexamethasone.
Typical dosing for postoperative inflammation is one drop four times daily for the first week, then tapering over two weeks. Because the molecule is relatively gentle on the trabecular meshwork, many ophthalmologists prefer it for patients with a history of glaucoma.
Common Alternatives
The market offers several steroid and non‑steroid drops that address the same problem. Below are the first‑time definitions of each, complete with their key attributes.
Prednisolone acetate is a high‑potency corticosteroid (1 % suspension) that penetrates the anterior chamber quickly, making it a go‑to for severe uveitis.
Loteprednol etabonate is a soft‑steroid formulated at 0.5 % concentration. Its ester bond breaks down rapidly in ocular tissue, delivering anti‑inflammatory action with a markedly reduced risk of IOP elevation.
Dexamethasone ophthalmic is a potent synthetic steroid (0.1 % solution) often used for macular edema and post‑cataract inflammation.
Ketorolac is a non‑steroidal anti‑inflammatory drug (NSAID) at 0.5 % that inhibits prostaglandin synthesis, providing pain relief without steroid‑related pressure spikes.
Ciprofloxacin is a broad‑spectrum fluoroquinolone antibiotic (0.3 % solution) frequently combined with steroids to prevent bacterial infection after surgery.
Two of the most common underlying conditions that drive the need for these drops are uveitis, an inflammation of the uveal tract that can threaten vision if untreated, and allergic conjunctivitis, an IgE‑mediated response causing itching, redness, and watery discharge.
Side‑by‑Side Comparison Table
| Drop | Potency (relative) | Typical dosing | Cost (USD per bottle) | IOP risk |
|---|---|---|---|---|
| FML Forte (Fluorometholone) | Medium | 1‑4× daily, taper 2‑3weeks | 15‑20 | Low |
| Prednisolone acetate | High | 1‑4× daily, taper 4‑6weeks | 25‑30 | Moderate‑High |
| Loteprednol etabonate | Medium‑Low | 1‑4× daily, taper 1‑2weeks | 20‑25 | Very Low |
| Dexamethasone ophthalmic | High | 1‑4× daily, taper 2‑3weeks | 22‑27 | Moderate |
| Ketorolac (NSAID) | Low (non‑steroid) | 1‑4× daily, 4‑6weeks | 12‑18 | None |
Decision Criteria: Which Drop Fits Your Needs?
- Potency vs safety: High‑potency steroids (prednisolone, dexamethasone) are best for aggressive uveitis but carry a higher IOP risk.
- Duration of therapy: Short‑course postsurgical inflammation often calls for medium‑potency, fast‑acting agents like FML Forte or loteprednol.
- Cost considerations: Generic fluorometholone and ketorolac tend to be the most budget‑friendly options.
- Preservative content: Patients with dry eye benefit from preservative‑free formulations, which are now available for fluormetholone and loteprednol.
- Comorbidity: If you have glaucoma, choose a drop with a very low IOP‑raising profile - loteprednol or fluormetholone are usually safest.
Practical Tips and Safety Measures
Regardless of the brand you pick, follow these simple habits to minimise complications:
- Wash hands thoroughly before each application.
- Avoid touching the tip of the bottle to the eye or eyelashes.
- Use a clean finger to pull down the lower eyelid and instil the drop without squeezing the bottle.
- Monitor your vision for any sudden blurring or halos - these could signal a pressure rise.
- Schedule a follow‑up eye exam within 1‑2weeks of starting a steroid, especially if you have a history of cataract or glaucoma.
Children and pregnant patients require extra caution. Fluorometholone’s low systemic absorption makes it a reasonable choice in pregnancy, but always consult your ophthalmologist first.
Related Concepts and Next Steps
Understanding the broader picture helps you make a more informed choice. Ocular inflammation can stem from infections, trauma, autoimmune disease, or postoperative healing. Mastering the distinction between sterile inflammation (where steroids excel) and infectious causes (where antibiotics are needed) prevents misuse.
If you want to dive deeper, consider reading about:
- The pharmacokinetics of ophthalmic corticosteroids.
- How preservative‑free eye drops improve comfort for dry‑eye sufferers.
- Emerging soft‑steroid molecules beyond loteprednol.
These topics sit in the same knowledge cluster, linking the current comparison to a larger conversation about safe, effective eye care.
Frequently Asked Questions
Can I use FML Forte if I have glaucoma?
Fluorometholone is known for a comparatively low tendency to raise intra‑ocular pressure, making it one of the safer steroid options for glaucoma patients. However, regular IOP checks are still essential, and your doctor may start with the lowest effective dose.
How does loteprednol differ from fluorometholone?
Loteprednol is a “soft” steroid designed to break down quickly after it exerts its anti‑inflammatory effect. This rapid metabolism translates into an even lower IOP‑raising risk than fluorometholone, though its potency is slightly less. It’s a good pick for patients who need extended use.
When should I choose an NSAID drop like ketorolac instead of a steroid?
If the inflammation is mild, pain‑dominant, or you have a known steroid response, an NSAID offers decent relief without affecting eye pressure. NSAIDs are also ideal after cataract surgery when used alongside a short‑course steroid.
Is it safe to combine fluormetholone with ciprofloxacin?
Yes. Many surgeons prescribe a combo bottle that contains both a steroid and an antibiotic to prevent postoperative infection while controlling inflammation. The two agents act through different mechanisms and do not interfere with each other.
How long can I stay on fluorometholone?
Typically, a course lasts 2‑3weeks, followed by a taper. Prolonged use beyond 6weeks increases the risk of cataract formation and IOP rise, so any extended therapy should be closely monitored by an eye specialist.
Cherish Capps
September 27, 2025 AT 13:05Fluorometholone’s low IOP risk is a good option for folks with glaucoma, even if you misspell the name sometimes.
Amy Carpenetti
September 29, 2025 AT 20:35The comparison chart nicely balances cost and safety, so readers can match a drop to their budget and health profile.
Paul Griffin
October 2, 2025 AT 04:05When choosing an ophthalmic anti‑inflammatory, it is advisable to prioritize agents with demonstrated low intra‑ocular pressure elevation, such as fluorometholone, especially in patients with pre‑existing glaucoma.
Michael Tekely
October 4, 2025 AT 11:35From a pharmacodynamic perspective, FML offers medium potency with a favorable safety margin, making it suitable for postoperative regimens without excessive IOP concerns.
Oscar Taveras
October 6, 2025 AT 19:05It is encouraging to see evidence‑based guidance that integrates both clinical efficacy and patient affordability 🙂.
katie clark
October 9, 2025 AT 02:35One must acknowledge the nuanced pharmacokinetic superiority of fluorometholone over its contemporaries, a distinction often overlooked by the lay practitioner.
Carissa Engle
October 11, 2025 AT 10:05Fluorometholone stands as a medium potency corticosteroid whose mechanism involves binding intracellular glucocorticoid receptors and suppressing pro‑inflammatory gene transcription. Its fluorine substitution enhances corneal penetration while mitigating mineralocorticoid activity. This biochemical profile translates into a lower propensity for intra‑ocular pressure elevation compared with older steroids. Patients who have a history of glaucoma therefore benefit from its relative safety. The typical dosing schedule of one drop four times daily for the initial week provides adequate anti‑inflammatory coverage. Tapering over subsequent weeks reduces the risk of rebound inflammation. Clinical studies have demonstrated comparable efficacy to higher potency agents in postoperative settings. Cost considerations further favor fluorometholone as it remains one of the most affordable generics available. The preservative‑free formulations improve tolerability for dry‑eye sufferers. Monitoring IOP remains essential even with low‑risk steroids. Ophthalmologists often select fluorometholone as a first‑line agent in mild to moderate inflammation. Its side effect profile includes a minimal risk of cataract formation when used short term. Long‑term use beyond six weeks may still pose cumulative risks. Patient education on proper drop instillation reduces contamination risk. Follow‑up visits within one to two weeks allow timely detection of any pressure spikes. Overall fluorometholone offers a balanced approach to efficacy, safety, and affordability.
Dervla Rooney
October 13, 2025 AT 17:35Fluorometholone provides a reasonable compromise between anti‑inflammatory potency and intra‑ocular pressure safety, making it an appropriate choice for many postoperative patients.
Johnny Ha
October 16, 2025 AT 01:05They don’t tell you how the big pharma lobby pushes the high‑potency steroids because it keeps the profit margins soaring while the quiet guys get stuck with cheap FML.
Mary Cautionary
October 18, 2025 AT 08:35The stratified assessment of therapeutic indices underscores fluorometholone’s advantageous positioning within the contemporary armamentarium of ocular anti‑inflammatories.
Crystal Newgen
October 20, 2025 AT 16:05Looks like a solid middle ground for people who don’t want to fry their eyes or their wallets.
Hannah Dawson
October 22, 2025 AT 23:35While the data suggest a lower IOP risk, the omission of long‑term safety endpoints raises questions about the robustness of the comparative analysis.
Julie Gray
October 25, 2025 AT 07:05It is incumbent upon the discerning clinician to scrutinize the underlying sponsorship of ophthalmic research, for undisclosed affiliations may subtly bias the presented superiority of fluorometholone.
Lisa Emilie Ness
October 27, 2025 AT 13:35Fluorometholone works well for short term inflammation with low cost
Emily Wagner
October 29, 2025 AT 21:05Think of eye drops like tools in a toolbox; fluorometholone is the reliable screwdriver that gets the job done without breaking the screws.
Mark French
November 1, 2025 AT 04:35I appreciate the practical tip about cost and safety; it’s helpful especially for patients navigating insurance limits.
Daylon Knight
November 3, 2025 AT 12:05Sure, because we all know “budget‑friendly” automatically means “best clinical outcome,” right?