How to Know If Your Supplement Is Safe with Your Medications
 Dec, 25 2025
Dec, 25 2025
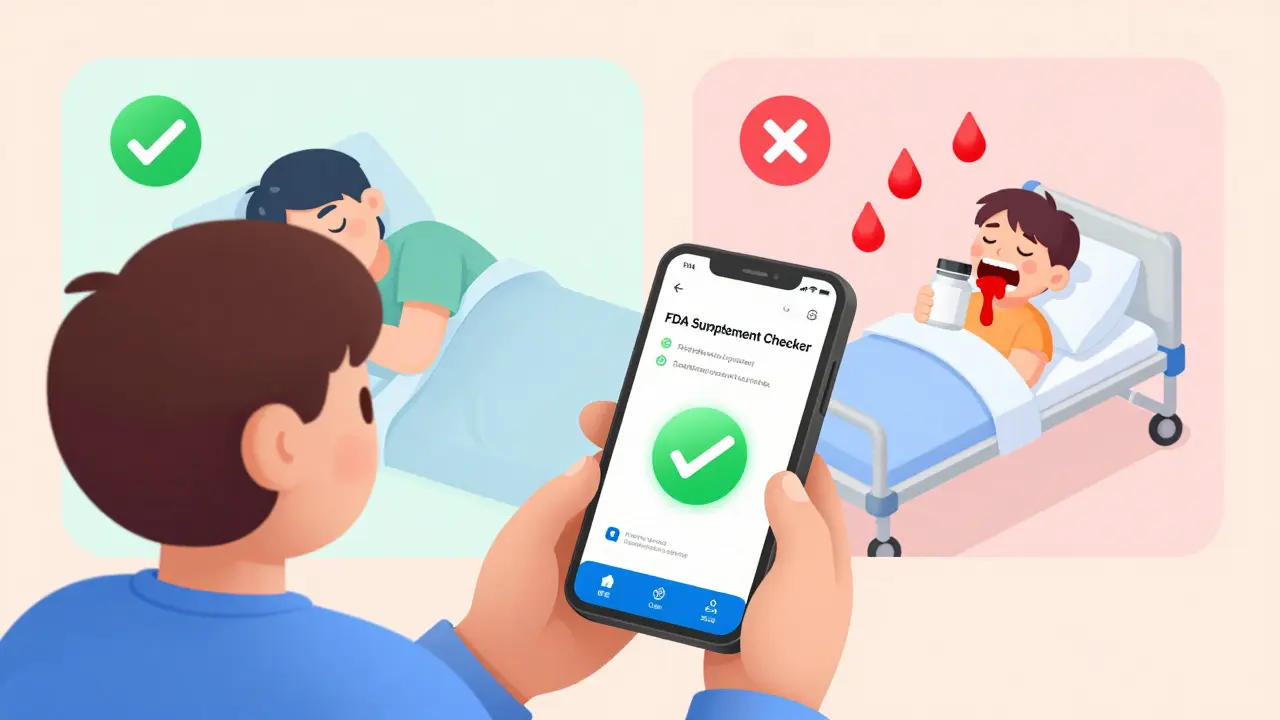
Every year, more than 23,000 people in the U.S. end up in the emergency room because a supplement they took messed with their prescription medication. And most of them had no idea it could happen. Just because something is labeled "natural" doesn’t mean it’s harmless-especially when you’re already on medicine.
You might be taking fish oil for your heart, vitamin D for your bones, or St. John’s wort for your mood. But if you’re also on blood thinners, antidepressants, or heart meds, you could be putting yourself at serious risk. The problem isn’t rare. It’s common. And it’s often invisible until something goes wrong.
Why Supplements Can Be Dangerous with Medications
Supplements don’t work like candy. They’re active substances that interact with your body’s chemistry-just like drugs. Many affect how your liver processes medications. One enzyme system, called cytochrome P450, handles about 60% of all prescription drugs. Some supplements can block it, others speed it up. Either way, your medication doesn’t work the way it should.
Take St. John’s wort, for example. It’s one of the most popular herbal supplements for mild depression. But it can slash the effectiveness of birth control pills by up to 50%, making pregnancy a real risk. It can also drop cyclosporine levels in transplant patients by half-enough to trigger organ rejection. And it doesn’t just affect one drug. It interferes with over 57 prescription medications, including antidepressants, heart drugs, and HIV treatments.
Even something as simple as calcium or iron can cause trouble. These minerals compete for the same absorption spots in your gut. If you take an iron supplement right after your thyroid medication, your body might not absorb enough of either. That means your thyroid levels stay out of range, and your anemia doesn’t improve.
The High-Risk Supplements You Need to Watch
Not all supplements are equal when it comes to danger. Some are mostly safe. Others are ticking time bombs when mixed with common meds.
- St. John’s wort: Highest risk. Avoid completely if you’re on antidepressants, birth control, blood thinners, or transplant meds.
- Ginkgo biloba: Safe for most people, but deadly with warfarin, Eliquis, or other blood thinners. It can double your risk of internal bleeding.
- Vitamin E (400 IU or more): Raises INR levels in people taking warfarin. That means more bruising, nosebleeds, even brain bleeds.
- Garlic, ginger, and fish oil: All thin the blood. If you’re scheduled for surgery, stop these at least a week before.
- Goldenseal: Blocks liver enzymes that break down many drugs. Can cause toxic buildup of medications like metformin or statins.
On the other hand, supplements like milk thistle, cranberry, and American ginseng have very few documented interactions. That doesn’t mean they’re risk-free-but they’re far safer.
What Your Doctor Won’t Always Ask
Most doctors focus on your prescriptions. They rarely ask about vitamins, herbs, or protein powders. And many patients don’t think to mention them. A 2023 survey found that 68% of people who take supplements never tell their doctor.
Why? Because they assume supplements are harmless. Or they think their doctor doesn’t care. Or they’re embarrassed. But here’s the truth: if you’re on more than one medication, your supplement list is just as important as your prescription list.
Doctors who follow updated guidelines now screen for supplement use during every medication review. The American Medical Association made this a standard in June 2023. But if your doctor hasn’t asked, don’t wait for them. Bring it up.

The Brown Bag Method: A Simple Way to Stay Safe
One of the most effective tools is called the "brown bag method." It’s exactly what it sounds like: take everything you’re taking-pills, capsules, powders, teas-and put it in a brown paper bag. Bring it to your next doctor or pharmacist appointment.
Studies show this cuts medication errors by 37%. Why? Because people forget things. They don’t remember the name of that herbal tea they started last month. They think the 500 mg of vitamin C is "too small to matter." But when it’s all laid out on the counter, patterns show up.
Pharmacists are trained to spot interactions. In 2021, Walgreens started requiring pharmacists to screen every customer’s supplement list. They found dangerous conflicts in 18% of cases. One woman was taking ginkgo with Eliquis. She didn’t realize it was causing her gums to bleed. Another man was mixing St. John’s wort with his antidepressant-leading to serotonin syndrome, a potentially fatal condition.
How to Check for Interactions Yourself
You don’t have to wait for an appointment. There are free, reliable tools you can use right now.
- Drugs.com Interaction Checker: Type in your medication and supplement. It gives you a risk level and explains what could happen.
- MedlinePlus: Run by the National Institutes of Health. Look up any supplement and check the "Interactions" section.
- Supplement labels: Read them. Look for warnings like "Do not take with blood thinners" or "May interfere with antidepressants." If it’s not there, that doesn’t mean it’s safe-just that the manufacturer isn’t required to say.
Also, check the active ingredients. Many multi-vitamins contain iron, calcium, or vitamin E. If you’re also taking separate supplements, you might be doubling up without realizing it.
When to Stop Taking a Supplement
Some supplements need to be paused before surgery, dental work, or even a routine procedure. Garlic, ginkgo, fish oil, and vitamin E can all increase bleeding risk. Most surgeons ask patients to stop them 7 to 10 days before surgery.
If you’re scheduled for any procedure-big or small-tell your provider what you’re taking. Even if they don’t ask, tell them anyway. It’s your body. You’re the one who knows what’s in it.
What’s Changing in 2025
Things are starting to improve. In late 2024, the FDA launched a new mobile app called the Dietary Supplement Ingredient Database. You can scan a supplement label, and it instantly tells you if it interacts with any of your medications. It’s free, easy to use, and available in English and Spanish.
Electronic health records are also starting to include supplement data. As of January 2024, 15% of U.S. hospitals now flag supplement-drug conflicts automatically when a doctor writes a prescription.
But until every pharmacy and doctor’s office has this built in, you’re still your own best defense.
What to Do Today
You don’t need to stop all supplements. You just need to be smart.
- Make a list of every supplement you take-including dosage and how often.
- Do the same for every prescription and over-the-counter drug.
- Use Drugs.com or MedlinePlus to check each one.
- Bring your list to your next appointment-even if it’s just for a cold.
- If you’re on warfarin, antidepressants, birth control, or transplant meds, assume any new supplement is risky until proven safe.
It’s not about fear. It’s about control. You’re already taking steps to care for your health. Don’t let a supplement undo that.
Can I take vitamin D with my blood pressure medication?
Yes, vitamin D is generally safe with most blood pressure medications. It doesn’t interfere with how those drugs work. But if you’re taking calcium supplements along with vitamin D, you should monitor your calcium levels. High calcium can affect heart rhythm and kidney function, especially in people with kidney disease. Always tell your doctor if you’re taking both.
Is it safe to take melatonin with antidepressants?
Melatonin is usually safe with most antidepressants, but not all. If you’re taking SSRIs like sertraline or fluoxetine, melatonin may increase drowsiness or affect your mood. In rare cases, it can contribute to serotonin syndrome when combined with certain antidepressants. Talk to your doctor before combining them, especially if you’ve had mood changes or sleep issues.
Do I need to stop my supplements before surgery?
Yes, you should. Supplements like garlic, ginkgo, fish oil, vitamin E, and ginger can increase bleeding risk. Most surgeons ask patients to stop them 7 to 10 days before surgery. Even if your doctor doesn’t mention it, bring your supplement list to your pre-op appointment. Better safe than sorry.
Can St. John’s wort affect my birth control?
Yes, it can. St. John’s wort speeds up how your body breaks down hormones in birth control pills, patches, and rings. This can drop hormone levels enough to cause ovulation-and pregnancy. Even if you’ve been on birth control for years, adding St. John’s wort can make it fail. Avoid it completely if you’re using hormonal contraception.
Why don’t supplement labels warn about drug interactions?
Because they’re not required to. Under U.S. law, supplements are treated like food, not drugs. Manufacturers don’t need FDA approval before selling them, and they don’t have to prove safety or list interactions. That’s why you can’t rely on the label alone. Always check with a pharmacist or use a trusted online tool like Drugs.com.
Final Thought: Your Health Is Your Responsibility
Supplements aren’t the enemy. But they’re not harmless either. The same caution you use with prescription drugs should apply to everything you put in your body. If you’re on medication, treat every supplement like a potential wildcard. Ask questions. Check for interactions. Bring your list to your appointments. Don’t assume it’s safe just because it’s natural. The truth is simple: natural doesn’t mean safe. And when it comes to your health, that’s the only rule you need to remember.
Jay Ara
December 25, 2025 AT 21:14ive been taking fish oil and lisinopril for years never thought twice about it until my cousin almost went to er over ginkgo and warfarin
now i just throw everything in a bag and show my dr
simple as that
Kuldipsinh Rathod
December 27, 2025 AT 01:29st johns wort messed with my antidepressants and i didnt even know it
felt like my brain was melting for a week
learned the hard way
SHAKTI BHARDWAJ
December 27, 2025 AT 08:03oh please like your doctor actually cares
they dont even know what ashwagandha is
and dont get me started on pharmacists who just scan barcodes and say "its fine"
youre on your own
and yes i take 12 supplements and 7 meds and im still standing
so sue me
also i dont trust anything that doesnt have a dragon on the label
Jeanette Jeffrey
December 28, 2025 AT 01:12the real issue here isnt supplements
its the delusional belief that natural = safe
arsenic is natural
botulinum toxin is natural
your body is a chemical reactor
and youre treating it like a smoothie bar
if you cant handle the complexity of your own biochemistry
maybe dont take anything at all
and yes i have a phd in pharmacology
Shreyash Gupta
December 29, 2025 AT 10:12just checked my supplement list
took fish oil and vitamin e
and im on a beta blocker
oh god
im gonna die
😭
im deleting everything
except my protein powder
that one’s fine right??
Ellie Stretshberry
December 29, 2025 AT 10:41my grandma took turmeric with her blood thinner and her knuckles turned purple
she thought it was "just anti-inflammatory"
took her three months to recover
now she brings her brown bag every visit
even the herbal tea she swears is "harmless"
turns out it had ginger in it
we all need to stop assuming
Zina Constantin
December 30, 2025 AT 06:05as a nurse in a rural clinic
i see this every single week
people think because its from a store
or its in a bottle with fancy letters
it cant hurt
but the truth
is that the most dangerous thing in their medicine cabinet
is often the one they never told anyone about
so yes
bring the brown bag
and dont be shy
Dan Alatepe
January 1, 2026 AT 05:59in nigeria we say "if it dont come from the hospital
it dont come from the gods"
but now everyone importing ginseng and moringa from china
and popping it like candy
my cousin took melatonin with his antidepressants
woke up screaming at the ceiling
thought he saw angels
turns out it was serotonin syndrome
he’s fine now
but he still takes it
and says "it helps my dreams"
weird people
Angela Spagnolo
January 2, 2026 AT 02:47i read this whole thing...
and then i cried...
because i realized i’ve been taking calcium with my thyroid med for 5 years...
and i never thought to space them out...
and i’ve been so tired...
and my hair has been falling out...
and now i feel so stupid...
but also... relieved?
thank you for writing this...
...i’m going to the pharmacy tomorrow...
carissa projo
January 3, 2026 AT 10:46the idea that we’re all supposed to be pharmacists now is exhausting
but also... necessary
we’ve been sold this myth that wellness is about adding more
when really it’s about knowing what to leave out
and when to say no
and when to ask for help
your body isn’t a lab experiment
it’s your home
and you wouldn’t let a stranger remodel your kitchen without asking questions
why treat your biology any differently?
Jody Kennedy
January 5, 2026 AT 05:04my doctor asked me about supplements once
i said "just vitamin d"
he looked at me like i’d lied about my name
then pulled up my chart
and said "you’re on 37 different things"
turns out i forgot my magnesium
and my zinc
and the probiotic i took for two weeks
and the chamomile tea
and the turmeric capsule i thought was "just a spice"
so now i have a spreadsheet
and a photo of my cabinet
and i never lie again
christian ebongue
January 6, 2026 AT 05:26so you’re telling me i’ve been taking garlic with warfarin for 3 years
and i’m still alive
huh
guess i’m just lucky
or maybe the FDA is just slow
or maybe this whole thing is fearmongering
...but i’ll still stop it before surgery
just in case
Alex Ragen
January 6, 2026 AT 23:58the tragic irony of modern health culture
is that we’ve replaced pharmaceutical authority
with supplement mysticism
and now we’re all amateur pharmacologists
while the real science
is buried under influencer testimonials
and amazon reviews
and instagram detox challenges
we’ve outsourced our biological autonomy
to the algorithm
and now we’re surprised when it breaks us
Lori Anne Franklin
January 8, 2026 AT 17:51just did the brown bag thing
found 4 things i forgot i was taking
including that ginseng tea from my aunt
who said it was "good for energy"
turns out it was messing with my blood pressure med
who knew??
thanks for the reminder
i feel smarter already