How to Participate in Patient Registries for Drug Safety
 Jan, 10 2026
Jan, 10 2026
When you start a new medication, especially one with known risks, your doctor might mention a patient registry. It sounds bureaucratic, maybe even intimidating. But here’s the truth: patient registries for drug safety are one of the most important tools we have to catch side effects that clinical trials miss. They’re not about research for scientists-they’re about protecting you.
Why Patient Registries Matter
Clinical trials are great, but they’re limited. They usually involve a few thousand people over months or a couple of years. Real life? Millions of people take the same drug for years, sometimes decades. Some side effects only show up in rare cases-or after long-term use. That’s where registries come in. Think of a registry like a living database. Every time someone takes a specific medication, their data-age, dosage, health history, side effects-is collected. Over time, patterns emerge. If 10 people on a new drug develop a rare liver issue, that’s a red flag. Without registries, those signals get lost in the noise. The FDA and European Medicines Agency now require safety registries for many high-risk drugs. In the U.S., 47 medications currently need mandatory registry enrollment. These include drugs like Tysabri for multiple sclerosis, Gilenya, and clozapine for schizophrenia. These aren’t optional. If you’re prescribed one of these, you can’t get the medication unless you’re registered.Types of Registries You Might Encounter
Not all registries are the same. There are four main types:- Disease registries track everyone with a specific condition, no matter what treatment they’re on. Think cystic fibrosis or Huntington’s disease registries.
- Product registries follow only people taking a specific drug. These are the ones tied to safety monitoring.
- Health services registries track people who’ve had certain procedures, like joint replacements or bariatric surgery.
- Exposure registries monitor people who’ve been exposed to something risky-like a chemical or a new medication during pregnancy.
How to Find Out If You Need to Join
You won’t always be told upfront. Sometimes, your pharmacy won’t fill your prescription until you’ve registered. Other times, your doctor’s office will send you paperwork. But you can check yourself. Go to the FDA’s Drugs@FDA database. Search for your medication. If there’s a required registry, it’ll say so under “Risk Evaluation and Mitigation Strategy” or REMS. In Europe, check the EMA’s product information page. You can also search ClinicalTrials.gov. Filter for “post-marketing” or “safety monitoring.” There are over 2,800 active registries listed there. Or, reach out to disease advocacy groups. The National Organization for Rare Disorders (NORD) connects patients to 147 registries for rare conditions.What Happens When You Join
Joining is usually simple. You’ll sign a consent form-often digital now-that explains what data will be collected and how it’s used. You’ll give basic info: name, date of birth, diagnosis, and current medications. Some registries ask for lab results or doctor visits. Others just want you to fill out a short survey every few months. The key thing to know: you’re not signing up for a clinical trial. You’re not getting experimental treatment. You’re helping make the drug safer for everyone. Data collection varies. Some registries use electronic health records (EHRs) to pull info automatically. Others rely on you reporting side effects via a website or app. The FDA wants at least 85% of critical safety data to be complete. That means they’re serious about accuracy.Voluntary vs. Mandatory Registries
There’s a big difference between mandatory and voluntary registries. Mandatory ones are tied to the drug’s approval. You can’t get the medicine without enrolling. These have high participation-up to 98% in cases like the UK’s clozapine registry. But they only capture people using the drug exactly as approved. Off-label use? That’s invisible. Voluntary registries are open to anyone. They’re great for capturing broader use, including people with other health problems or older adults. But they suffer from bias. People who join are often younger, healthier, and more tech-savvy. That means the data might not reflect the full picture. The FDA found that patients in voluntary registries are, on average, 7.3 years younger and have fewer chronic conditions than those who don’t join. That’s a gap. But even imperfect data is better than no data.Privacy and Your Data
This is the biggest concern for many people. Will your information be sold? Will your insurance find out? Registries are governed by strict rules. In the U.S., they must follow HIPAA. In Europe, GDPR applies. Your name and identifying details are stripped from the data before it’s shared with drug companies or regulators. Researchers see codes, not names. A 2022 survey found that 41% of people didn’t join registries because they were afraid of privacy breaches. But registries don’t share data with insurers, employers, or marketers. The data is used only for safety analysis. Some newer platforms, like MyDataCan, let you control who sees your information. You can choose to share with researchers, your doctor, or keep it private. This kind of control is becoming more common.How Long Do You Have to Stay In?
It depends on the drug. For short-term medications, you might only be in for a year. For chronic conditions like multiple sclerosis or rheumatoid arthritis, registries can last decades. The average person stays in a registry for about 2.7 years. But dropout rates are high-nearly 19% each year. Why? People forget. They move. They feel like it’s not worth it. That’s why the best registries reach out. They send reminders. They send newsletters with updates on what the data is showing. Some even offer free transportation to follow-up visits. If you’re asked to join, don’t ghost it. Even a few check-ins help.What’s in It for You?
You might think: “I’m giving data, but what do I get?” Many participants say they feel more in control. A 2022 survey of over 1,200 registry users found that 68% learned something new about their condition. Over half said they had better conversations with their doctors because of the registry. For rare diseases, registries can be life-changing. The Elaprase registry for Hunter syndrome helped get approval for treatment in children under six-because the registry proved it was safe. That’s real impact. You’re not just a data point. You’re part of a system that prevents future harm. If a new side effect shows up, your data might help stop it before it hurts someone else.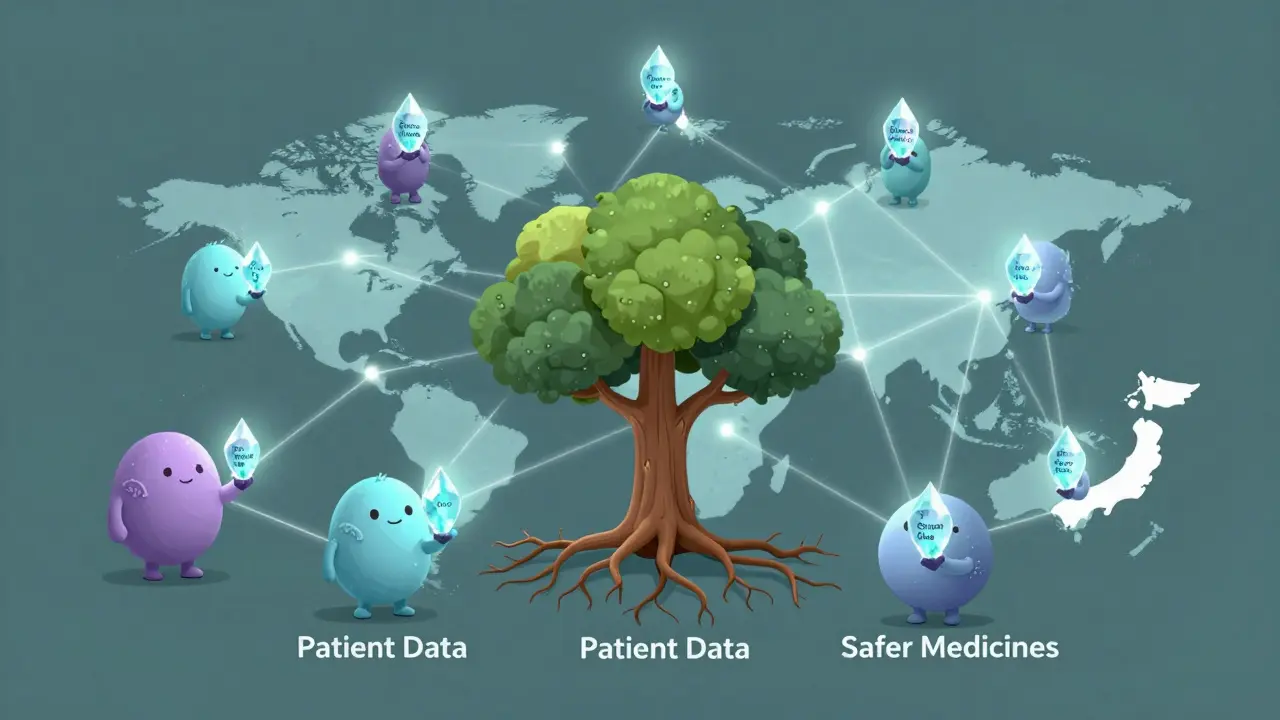
What If You Don’t Want to Join?
If a registry is mandatory and you refuse, you won’t get the medication. That’s the law. But you can ask questions. Ask your doctor: Why is this required? What data will be collected? How is it protected? If it’s voluntary, you’re free to say no. But consider this: if you’re on a drug with serious risks, your silence makes it harder to spot problems. Someone else might be affected next.What’s Changing in 2025?
The rules are getting stricter-and better. By 2025, the FDA will require all new drug applications with serious risks to include a registry plan. That means more patients will be enrolled. The FDA’s MyStudies app lets you report side effects directly from your phone. Over 140,000 people are already using it. Soon, 83% of patients on high-risk drugs will be automatically enrolled through their electronic health records-unless they opt out. Blockchain pilots are testing secure, patient-controlled data sharing. And global standards are being set so registries in Ireland, the U.S., and Japan can talk to each other. This isn’t science fiction. It’s happening now.What You Can Do Today
1. Ask your doctor if your medication requires a registry. Don’t wait for them to bring it up. 2. Check Drugs@FDA or the EMA website if you’re unsure. 3. Join if asked. Even if it’s a simple survey, your input matters. 4. Update your info. If your health changes, let the registry know. 5. Ask for updates. Most registries send out summaries of what they’ve learned. Read them. You don’t need to be a scientist or a tech expert. You just need to care about safety-for yourself and for others.Are patient registries the same as clinical trials?
No. Clinical trials test new treatments under controlled conditions. Patient registries collect real-world data from people already taking approved medications. You’re not getting an experimental drug-you’re helping monitor its safety over time.
Can I leave a registry after I join?
Yes. You can withdraw at any time. Your data may still be used if it was collected before you left, but you won’t be contacted again. The registry must honor your request immediately.
Will joining a registry affect my insurance or employment?
No. Registries are required to remove your personal details before sharing data. Your information is protected by HIPAA in the U.S. and GDPR in Europe. Insurance companies and employers cannot access your registry data.
What if I don’t have internet access or a smartphone?
Most registries still offer paper forms, phone surveys, or in-person check-ins. If you’re enrolled, ask your doctor’s office or the registry coordinator about alternative ways to participate. You don’t need technology to help.
How do I know if a registry is legitimate?
Legitimate registries are run by hospitals, government agencies (like the FDA or EMA), or trusted patient advocacy groups. Check the website’s domain-it should end in .gov, .edu, or be linked from your doctor’s office. Never give personal details to a registry you didn’t hear about from a healthcare provider.
Jennifer Phelps
January 11, 2026 AT 15:22So if I'm on Tysabri I literally can't get my script filled unless I sign some form? That's wild. I thought my doctor was just being extra but turns out it's the law. I didn't even know this existed until now.
Sona Chandra
January 12, 2026 AT 15:44THIS IS WHY PEOPLE DIE. I knew a girl who got liver failure on that clozapine thing and no one knew until it was too late because NO ONE WAS TRACKING. Now they make you sign up but what if you're poor and don't have a phone or internet? They don't care. They just want their data.
beth cordell
January 12, 2026 AT 18:04OMG I just joined the Gilenya registry last week 😭 I thought it was just another form but now I get it. They sent me a cute little update last month about how 3 people had a weird reaction and now doctors are warning others. Feels kinda powerful?? 🤍
Lauren Warner
January 14, 2026 AT 11:15Let's be real. These registries are corporate liability shields disguised as patient safety. The FDA doesn't care about you. They care about avoiding lawsuits. If your data helps them avoid a recall, great. If it doesn't? You're just another entry in a spreadsheet.
Craig Wright
January 15, 2026 AT 17:25As a British citizen, I find it alarming that the US system mandates registry participation as a condition of prescription. In the NHS, patient consent is paramount. This feels like coercion dressed in medical jargon. The state should not compel participation in data collection under threat of denied treatment.
Lelia Battle
January 16, 2026 AT 06:01It’s interesting how we treat data as both sacred and disposable. We demand privacy from corporations but willingly give away our health history for the abstract good of ‘science’. Is it altruism or resignation? Maybe both. Either way, the system relies on our quiet compliance.
Rinky Tandon
January 16, 2026 AT 23:11Product registries are the only valid mechanism for pharmacovigilance. Disease registries are noise. Exposure registries are speculative. Health services registries are administrative overhead. If you're not tracking drug-specific adverse events in real-time with longitudinal data, you're not doing pharmacovigilance-you're performing performative medicine.
Ben Kono
January 17, 2026 AT 22:34I got the clozapine registry form and just threw it in the drawer. Who has time for this? I'm already seeing my doc every month. Why do I need to fill out another form every 3 months? It's just busywork.
Cassie Widders
January 18, 2026 AT 01:08I joined the MS registry last year. They sent me a letter last month saying they found a pattern with people over 50 having more fatigue. My doctor changed my dose because of it. Small thing. But it helped.
Konika Choudhury
January 18, 2026 AT 03:51Why should I trust American drug companies? They lie about side effects all the time. Now they want me to give them my data? No thanks. I'll take my chances.
Darryl Perry
January 19, 2026 AT 07:55Registries are mandatory for 47 drugs. That's not safety. That's control. If you're not compliant, you're not getting the med. That's not healthcare. That's institutional coercion.
Windie Wilson
January 20, 2026 AT 10:43So I'm supposed to feel like a hero for filling out a survey every 6 months? Meanwhile my insurance raised my premiums because I have 'chronic autoimmune condition'-which they got from... you guessed it, a registry. Thanks for the nobility, guys.
Daniel Pate
January 20, 2026 AT 23:25If registries are so vital, why is dropout so high? Why do people disengage? Because they’re not designed for humans. They’re designed for metrics. We’re not data points-we’re people with lives that get messy. The system ignores that.
Amanda Eichstaedt
January 21, 2026 AT 16:53I used to think these things were pointless. Then I got a message from the registry saying they’d spotted a new interaction between my med and a common OTC painkiller. My doctor changed my plan. That saved me from a hospital trip. So yeah. I’m in. Not for science. For me.
Jose Mecanico
January 21, 2026 AT 19:12I'm in two registries. One for my MS, one for my depression med. I fill out the surveys when I remember. I don't expect anything back. But I know someone else might benefit. That's enough.