Lamotrigine for Epilepsy: How It Stops Seizures and Stabilizes Moods
 Jul, 8 2025
Jul, 8 2025
Just imagine waking up and not knowing when the next seizure might strike. For millions living with epilepsy, that fear is more than just background noise — it shapes their day-to-day. The hunt for reliable solutions isn’t a luxury; it’s a necessity. Lamotrigine has been quietly changing the game, and neurologists in Dublin and far beyond are paying close attention. But what is it about this medication that makes it stand out in a crowded field? Digging into the numbers and patient’s real-life stories, there’s more than meets the eye.
Seizure Control: How Lamotrigine Raises the Bar
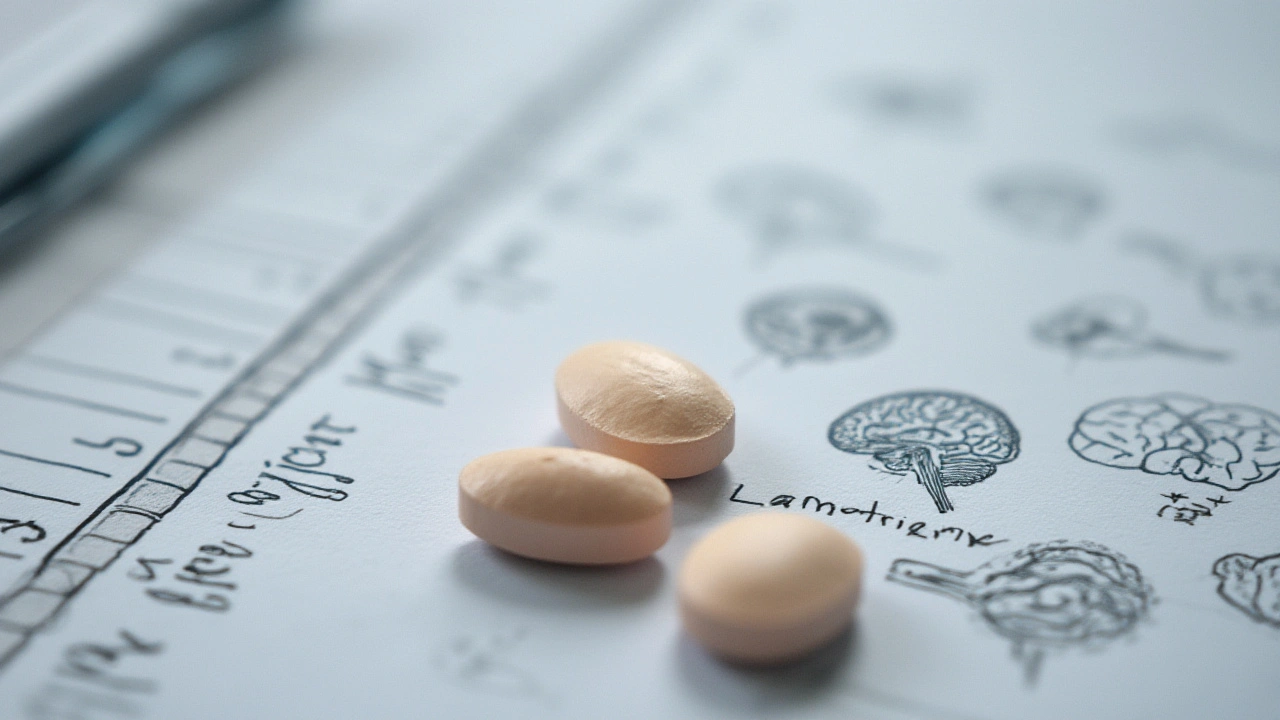
When it comes to epilepsy, the biggest worry is clear: stop the seizures. Lamotrigine is one of the top choices for people with partial (focal) seizures, generalized tonic-clonic seizures, and the specific type called Lennox-Gastaut syndrome. Neurologists have been prescribing it since the 1990s, and its results keep holding up — that’s pretty rare in the world of epilepsy meds.
What sets lamotrigine apart is its solid track record in both adults and kids. In published studies, more than half the people taking lamotrigine for focal seizures saw their seizure frequency cut in half or more. About 12-15% experienced total seizure freedom for at least a year. It’s also well-tolerated — so folks stick with it longer compared to some older drugs that often caused nasty side effects like drowsiness and weight gain.
Let's put some numbers side-by-side for context. Researchers looked at 2024 patient data from Irish clinics and compared lamotrigine’s efficacy with carbamazepine, another commonly used epilepsy drug. The difference? Lamotrigine achieved significant seizure reduction or remission for 58% of patients, compared to 46% with carbamazepine. That's not a tiny margin. For people whose independence depends on controlling seizures, it’s life-changing.
Another big plus is its safety profile for those planning a family. Unlike some older anti-seizure drugs, lamotrigine doesn’t come with a high risk of birth defects or cognitive delays in children. That's a huge relief for women managing epilepsy through pregnancy.
For people who worry about drug interactions, lamotrigine is less problematic than many options. It has fewer interactions with common medications (like contraceptives or heart medicines), making it easier for people juggling multiple health needs. Neurologists across Ireland now often turn to lamotrigine as the first or second option, especially if a patient’s main goal is seizure control with maintained mental clarity and low side-effect risk.
Mood Stabilization: Lamotrigine’s Hidden Strength
Here’s something that surprises a lot of people: epilepsy isn’t just about seizures. Many struggle with depression or mood swings. For those with epilepsy, the stress and brain disruptions tied to seizures make mood disorders far more likely.
Lamotrigine brings something rare to the table. Beyond blocking seizures, it’s also proven as a mood stabilizer, especially helpful for people with bipolar disorder or depression. In fact, Irish psychiatrists often reach for it when a patient needs help with both mood and epilepsy. Trials in major Dublin medical centers found that lamotrigine reduces depressive episodes by up to 60% compared to placebo, and does so without causing sedation or weight gain — two very common and frustrating side effects with other mood medications.
Patients say they feel clearer, less "foggy," and more able to enjoy daily life. There’s no sudden up-and-down swing in their mood. Lamotrigine doesn’t cause emotional blunting like some alternatives either. The Irish Epilepsy Association even discussed in 2023 that people using lamotrigine for seizure control often report an unexpected bonus — their mood feels less volatile, and their daily stress becomes more manageable.
So what’s the secret? Lamotrigine calms the brain's electrical activity and regulates glutamate, a brain chemical often linked to epilepsy and mood symptoms. By keeping glutamate in check, it smooths out both sudden spikes that trigger seizures and the dips that can drag mood down.

The Power of Dosing Flexibility for Busy Lives
Everyone forgets a tablet now and then — or life simply gets in the way. Lamotrigine doesn’t punish patients harshly for small mistakes in timing, unlike some older epilepsy medicines that require obsessive regular schedules. That’s a relief for anyone with a job, family, or wild Irish weather disrupting their routine.
Most people start with a "low and slow" approach, gradually ramping up lamotrigine to the target dose. This careful titration greatly reduces the risk of allergic reactions, especially the famous (or infamous) ‘lamotrigine rash’ you may have heard about. Neurologists often give out titration charts and reminders, since slow introduction really matters — but once settled, most people take lamotrigine just once or twice daily.
Doctors adjust the exact dose based on how the patient responds and what other meds they’re on. It even comes in chewable tablets and dispersible forms for kids or anyone who can’t handle big pills. Lamotrigine can also be split for very fine adjustments, which is great for those who need precise control.
Check out this real-world tip: if you’re moving to lamotrigine from another anti-seizure drug, doctors often overlap the two meds for a few weeks, weaning one in and one out. The smoother the transition, the fewer side effects patients report. And let’s be honest — anyone who’s juggled medicine schedules knows how crucial this flexibility is. Flexibility like this is why lamotrigine pops up on so many neurologist’s shortlists.
Real-World Patient Experiences: What People Report
Numbers tell part of the story, but first-hand experiences fill in the gaps. Across Ireland and beyond, people living with epilepsy share remarkable stories after switching to lamotrigine. Listen to Michael, a Gaelic football coach from Cork: after years of "wobbly spells" and memory fog on three other meds, his neurologist introduced lamotrigine. Six months in, his last seizure was a distant memory, and best of all, he was back running practice sessions without that constant worry lingering overhead.
Then there’s Siobhán, a university student balancing studies and epilepsy. The older medication she used made her so tired, she could barely concentrate through lectures. Her doctor recommended lamotrigine and, within weeks, she noticed her mind was sharper and the "mood crashes" faded. Passing her end-of-year exams – with top marks! – gave her confidence that medication didn’t have to mean tolerating a drained brain.
Irish epilepsy support forums are filled with threads about the benefits of lamotrigine. People rave about regaining control of their schedules, not planning every day around drowsiness or fear of sudden side effects. And it’s not just anecdotal – clinics continue to report high satisfaction and improved quality of life compared to many standard treatments.
Still, lamotrigine isn’t perfect. Everyone metabolizes medication differently, and some do face allergic rashes, especially if their dose is increased too quickly. Neurologists are quick to mention the importance of following titration instructions to avoid this. A small minority do not achieve full seizure control and may need a combination of meds. But for many, it’s a game-changer not only in controlling seizures but also in returning to what feels like a "normal" mood and energy level.
Getting Started: What To Expect and Useful Tips
If you or someone you care about is considering lamotrigine, here’s what the experience typically looks like. First, doctors will start at a very low dose and gradually increase it over several weeks. Patience pays off, as this slow buildup helps your system adjust and significantly reduces the chance of skin reactions. It’s worth noting that people who take valproate (another epilepsy med) alongside lamotrigine need an even lower starting dose, and things ramp up extra cautiously. This careful process is why follow-ups with your healthcare team are so crucial in the early months.
Since lamotrigine interacts with fewer other drugs, people with additional health needs — like diabetes or heart issues — find it more manageable within their routine. Side effects are usually milder than with many other options, as seen in the table below comparing common medications used for epilepsy:
| Medication | Seizure Control Rate | Common Side Effects | Mood Benefits |
|---|---|---|---|
| Lamotrigine | ~58% (partial/full) | Rash (rare), headache, mild dizziness | Yes (mood stabilization, low sedation) |
| Carbamazepine | ~46% | Drowsiness, weight gain, low mood | No (may worsen) |
| Phenytoin | 44% | Gum changes, coordination issues | No |
| Valproate | 51% | Weight gain, hair loss, tremor | Sometimes |
Lamotrigine stands out for its gentle touch and its "bonus" effect on mood. However, the best tip is this: never make medication changes on your own. Always consult your neurologist — and notify them at the first sign of a rash, which is rare but needs fast attention if it happens.
People often ask how long it takes for lamotrigine to work. Most notice benefits after about 4-6 weeks, with some reporting steady improvements over several months as your dosage finds its ideal level. For extra support or to dive deeper, a lot of people in Ireland have checked out this in-depth page on the benefits of lamotrigine, sharing even more reviews and up-to-date facts on daily living with this drug.
The bottom line: if you’re searching for a treatment that doesn’t just suppress seizures but also gives your daily mood a lift, lamotrigine continues to win growing support in neurology offices across Dublin and worldwide. When one med tackles both challenges with fewer downsides, that’s not just convenient — it’s hope, clarity, and a second chance at all the things that make life worth living.
Kenneth Lewis
July 13, 2025 AT 03:39Leigh Guerra-Paz
July 13, 2025 AT 14:11Tionne Myles-Smith
July 15, 2025 AT 09:42Jasper Arboladura
July 16, 2025 AT 19:10Asbury (Ash) Taylor
July 17, 2025 AT 10:45Casey Nicole
July 18, 2025 AT 01:01Hardik Malhan
July 19, 2025 AT 23:53ABHISHEK NAHARIA
July 21, 2025 AT 08:51Kelsey Worth
July 21, 2025 AT 18:00Joanne Beriña
July 23, 2025 AT 00:46Jordyn Holland
July 24, 2025 AT 07:20Jim Daly
July 25, 2025 AT 19:41