Managing Medication Allergies and Finding Safe Alternatives
 Jan, 7 2026
Jan, 7 2026
When you hear the word allergy, you probably think of pollen, peanuts, or pet dander. But what if your body reacts badly to a pill you took for a sore throat? Medication allergies are real - and they’re often misunderstood. Many people believe they’re allergic to penicillin because they got a rash as a child. But chances are, they’re not. And that mislabeling can cost you more than just time - it can put your health at risk.
What Is a True Medication Allergy?
A true drug allergy happens when your immune system mistakes a medication for a harmful invader. It’s not just a side effect. It’s not just feeling sick. It’s your body launching an immune response - sometimes violently. Symptoms can range from a mild rash to swelling, trouble breathing, or full-blown anaphylaxis, which can be deadly.Here’s the catch: only about 10% of people who say they’re allergic to penicillin actually have a real allergy. The rest may have had a side effect - nausea, diarrhea, or a harmless rash - and got labeled as allergic without proper testing. That label sticks. Even if you outgrew it. Even if you never had it to begin with.
According to the CDC, 90-95% of people with a penicillin allergy label can safely take penicillin after a proper evaluation. That’s not a guess. That’s data from skin tests and oral challenges done in clinics across the U.S. And yet, most people never get tested.
How to Know If It’s Really an Allergy
Not every bad reaction means allergy. Here’s how to tell the difference:- True allergy symptoms: Hives, swelling of lips or tongue, wheezing, drop in blood pressure, vomiting or diarrhea within minutes to hours after taking the drug.
- Side effects: Upset stomach, dizziness, headache, or a mild rash that doesn’t spread or worsen. These aren’t immune responses - they’re just how your body reacts to the chemistry of the drug.
Penicillin is the most common culprit. But sulfa drugs, NSAIDs like ibuprofen, and certain antibiotics are also frequent triggers. The key is documentation. If you’ve had a reaction, write down:
- The exact name of the drug (brand and generic)
- What happened - symptoms, timing, how long it lasted
- How many doses you took before the reaction
- How you took it - pill, injection, IV
- The date
This isn’t just for your records. It’s what doctors need to decide if you’re truly allergic or just unlucky with a side effect. The National Institute for Health and Care Excellence (NICE) says every provider must confirm your allergy status before prescribing anything. Too often, they don’t.
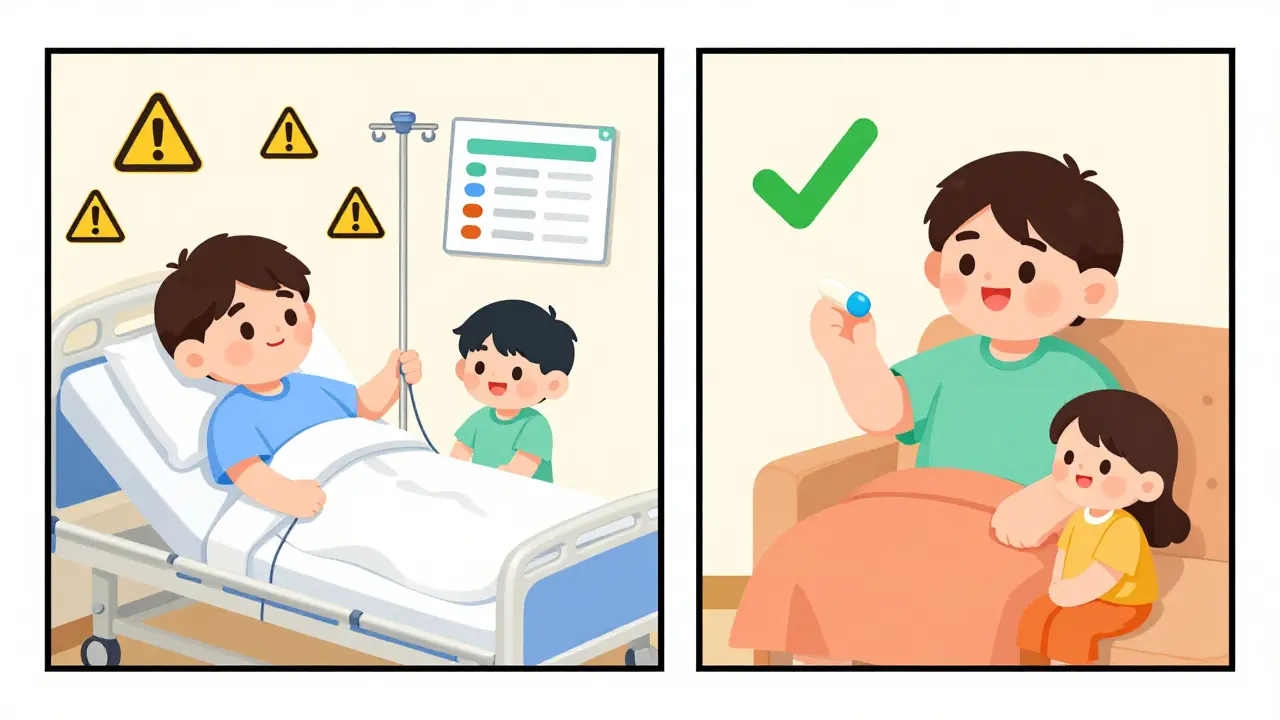
Why Mislabeling Is Dangerous
If you’re labeled allergic to penicillin - even incorrectly - doctors will avoid it. They’ll pick something else. But those alternatives aren’t better. They’re often:- More expensive - azithromycin can cost $25 for a 5-day course. Penicillin? Around $4.
- Broader-spectrum - they kill more types of bacteria, which increases antibiotic resistance.
- More likely to cause other problems - like Clostridium difficile infection, a severe gut illness that leads to longer hospital stays and higher death rates.
Studies show patients with a penicillin allergy label have a 40% higher chance of getting C. diff and stay in the hospital 30% longer. That’s not because penicillin is unsafe. It’s because the alternatives are riskier.
And here’s the worst part: if you’re allergic to penicillin and you need it - like for syphilis during pregnancy - you can’t just skip it. Penicillin is the only treatment that works. That’s when doctors turn to desensitization.
Desensitization: When You Need the Drug You’re Allergic To
Desensitization isn’t a cure. It’s a temporary workaround. You’re given tiny, increasing doses of the drug under close medical supervision - usually over several hours. Your immune system gets tricked into tolerating it for the duration of treatment.This works for about 80% of people with penicillin allergies when done by trained allergists. It’s used in hospitals for conditions like neurosyphilis, endocarditis, or severe infections where no other drug works.
But it’s not for everyone. If you’ve had anaphylaxis in the last 10 years, you won’t be desensitized in an outpatient clinic. The risk is too high. That’s why proper history matters. Not every rash means you’re high-risk.
Safe Alternatives to Penicillin
If you truly have a penicillin allergy, here are the most common alternatives - and what you should know about each:| Alternative | Typical Use | Pros | Cons |
|---|---|---|---|
| Azithromycin | Strep throat, pneumonia | Once-daily dosing, good for mild infections | Expensive, can cause stomach upset, increases antibiotic resistance |
| Doxycycline | Lyme disease, acne, urinary infections | Low cost, effective against many bacteria | Not for kids under 8 or pregnant women, can cause sun sensitivity |
| Levofloxacin | Severe lung or urinary infections | Strong coverage, oral and IV options | Risk of tendon rupture, nerve damage, not for long-term use |
| Cefdinir (cephalosporin) | Ear infections, sinusitis | Often tolerated by penicillin-allergic patients | Low cross-reactivity (under 5%), but still risky if you had anaphylaxis |
Important note: Third-generation cephalosporins like ceftriaxone have very low cross-reactivity with penicillin - less than 5%. Many doctors still avoid them out of habit. But modern guidelines say they’re often safe. Ask your doctor.
What You Can Do Right Now
If you’ve been told you’re allergic to a drug - especially penicillin - here’s what to do:- Check your records. Look at your medical chart. Is the allergy listed as "rash"? "Stomach ache"? That’s not a true allergy.
- Ask your doctor about testing. Skin tests and oral challenges are quick, safe, and covered by most insurance.
- Carry a wallet card. List your confirmed allergies, reactions, and dates. Update it after testing.
- Speak up at every appointment. Don’t assume your allergy is in the system. Say it. Write it. Show your card.
One patient in Dublin, 38, had a childhood rash after amoxicillin. For 20 years, she avoided all penicillin-type drugs. She got pneumonia last year and was given vancomycin - a powerful IV antibiotic. She spent five days in the hospital. After testing, she was cleared. Next time, she got penicillin at home. No hospital. No IV. No cost.

Where to Get Help
You don’t have to figure this out alone. Board-certified allergists specialize in drug allergies. In the U.S., the American Academy of Allergy, Asthma & Immunology has a tool to find one near you. In Ireland, your GP can refer you to an immunology clinic. The process usually takes one to two visits.There’s also a growing movement called "Choose Penicillin," launched in early 2023. It’s pushing hospitals and clinics to test and reclassify patients with old allergy labels. Pilot programs have cut unnecessary antibiotic use by 65%.
Health systems are starting to catch up. The CDC now recommends outpatient skin testing for low-risk patients. Electronic health records are being updated to capture detailed allergy data - not just "penicillin allergy," but exactly what happened, when, and how.
What’s Next
By 2027, half of all penicillin allergy evaluations are expected to happen in primary care clinics - not just allergy centers. That’s a big shift. It means more people will get tested, more people will be cleared, and fewer will be stuck with risky, expensive alternatives.The bottom line? If you’ve been told you’re allergic to a drug, don’t accept it as permanent. Ask questions. Get tested. Your next infection might be treated with a simple, cheap pill - not a hospital stay.
Can you outgrow a medication allergy?
Yes, especially with penicillin. Studies show up to 80% of people who had a penicillin allergy as children lose it over time - even if they never had a true IgE-mediated reaction. The immune system changes. What felt like an allergy at age 6 may be nothing at 30. Testing is the only way to know for sure.
Is a rash always a sign of a drug allergy?
No. Many rashes after taking antibiotics are not allergic. They’re often viral rashes that happen to appear while you’re on the drug. True allergic rashes are raised, itchy, and spread quickly. Non-allergic rashes are flat, not itchy, and may look like measles. A doctor can help tell the difference.
Can I take cephalosporins if I’m allergic to penicillin?
For most people, yes. Third-generation cephalosporins like ceftriaxone and cefdinir have a cross-reactivity rate of under 5% with penicillin. That’s much lower than old estimates. If your reaction was mild - like a rash - you’re likely safe. If you had anaphylaxis, your doctor will need to evaluate your risk carefully.
What if my allergy is still listed after I was cleared?
This is common. Medical records don’t always update automatically. You may need to bring your test results to every appointment. Ask your doctor to remove the old label and replace it with "allergy ruled out" or "no confirmed allergy." Keep a copy of your test report in your phone or wallet.
Are there any new treatments for drug allergies?
The biggest change isn’t a new drug - it’s better testing. Skin testing and oral challenges are now faster, safer, and available in more clinics. The FDA is also working on standardizing how drug allergies are recorded in electronic health records. By 2024, new rules may require doctors to document the type of reaction, not just the drug name. That will reduce mislabeling.
Manish Kumar
January 8, 2026 AT 07:47Man, this whole thing hits different when you think about it-how we just accept medical labels like they’re carved in stone, when really, our bodies are fluid, changing, evolving. I had a rash after amoxicillin at 7, got labeled allergic, and for 22 years I avoided anything even remotely penicillin-related. Turns out? My immune system just had a bad day. No anaphylaxis, no hives, just a stupid rash that looked like a toddler’s crayon drawing. I got tested last year-skin test took 20 minutes, oral challenge was me sipping sugar water with antibiotics in it while a nurse watched me like I was a bomb. I’m cleared now. Penicillin for my sinus infection last month? $4. No hospital. No IV. Just me, my bed, and a bottle of cheap antibiotics that actually worked. Why aren’t we doing this for everyone? Why do we treat medical labels like religious dogma instead of data points?
Aubrey Mallory
January 9, 2026 AT 12:40Let me be clear: if your doctor hasn’t asked you about your antibiotic allergy history with the precision of a forensic accountant, they’re doing you a disservice. This isn’t about being ‘overcautious’-it’s about systemic laziness masked as safety. I’ve seen patients die because they were given vancomycin instead of penicillin for syphilis during pregnancy. Vancomycin isn’t safer-it’s a sledgehammer. Penicillin is a scalpel. We’ve got the tools to test, we’ve got the data to prove it, and yet we keep treating patients like they’re walking liability risks instead of human beings with evolving biology. Stop guessing. Start testing. And if your provider won’t? Find one who will. Your life isn’t a gamble.
Prakash Sharma
January 11, 2026 AT 06:40India has the same problem-doctors write ‘penicillin allergy’ on charts like it’s a default setting. My cousin got labeled after a fever rash at 5. She’s 34 now, never had another reaction. Last year she got pneumonia and was given azithromycin-cost her 12,000 rupees. Penicillin would’ve been 400. She spent three days in the hospital. If they’d just tested her, she’d have been home in one. This isn’t just medical ignorance-it’s economic exploitation. Pharma companies don’t care if you’re allergic or not-they profit from the alternatives. And doctors? They’re too rushed to dig deeper. We need mandatory allergy re-evaluation every 10 years. Period. No more lazy labels.
Lois Li
January 12, 2026 AT 03:48I’m so glad someone wrote this. I’m a nurse in rural Oregon and I’ve seen this over and over. Patients come in with ‘penicillin allergy’ written in their chart and no details-just that phrase. No date, no symptoms, no context. I’ve had to push back on prescriptions because I knew the alternatives were worse. I started keeping a printed handout in my pocket-‘Penicillin Allergy: Myth vs. Reality’-and handing it to patients. Most have never heard of desensitization. Most think they’re doomed to expensive antibiotics forever. It’s heartbreaking. We need this info in every ER, every clinic, every pharmacy. Not just for patients-but for providers who never learned this in med school.
Joanna Brancewicz
January 14, 2026 AT 01:08True IgE-mediated reactions are rare. Most reactions are non-allergic. Cross-reactivity with cephalosporins is <5%. Penicillin remains first-line for syphilis, strep, and many infections. Testing is safe, cost-effective, and underutilized. CDC and NICE guidelines support this. Mislabeling increases C. diff risk by 40%. Avoiding penicillin increases antibiotic resistance. The data is clear.
Evan Smith
January 15, 2026 AT 18:36So let me get this straight… I spent 15 years avoiding penicillin because I got a rash after taking it when I was 8… and now you’re telling me I could’ve just taken a pill for my ear infection instead of getting a 3-day IV drip that cost me $2,000 and made me feel like a zombie? And the reason I didn’t know this is because… nobody told me? Wow. Just… wow. I feel like I was scammed by the medical system. Like I was handed a ‘beware of dog’ sign when I was 8 and nobody ever told me the dog was a golden retriever who just wanted belly rubs. Can we get a meme for this? ‘My doctor labeled me allergic to penicillin. My immune system just wanted a nap.’
Molly Silvernale
January 16, 2026 AT 08:45It’s funny-how we treat medicine like it’s a static code, when the human body is a living poem, constantly rewriting itself. That rash? A whisper from your immune system, not a scream. That nausea? Your gut saying ‘hey, this chemistry doesn’t sit right,’ not your soul rejecting the drug. We’ve turned medical history into a tombstone, when it should be a journal-editable, revisable, alive. I used to believe my penicillin label was sacred. Then I got tested. And now I see: labels aren’t truth-they’re echoes. And sometimes, the echo is just the sound of fear, repeating itself long after the original scream has faded. I’m not allergic anymore. I’m just… free.
christy lianto
January 17, 2026 AT 13:25I had a patient last week-68-year-old woman, told she was allergic to penicillin since she was 10. She’d been on clindamycin for every infection since. Got a UTI, ended up with C. diff, spent 17 days in the hospital. We tested her. Negative. She cried. Not from pain-from relief. She said, ‘I thought I was broken.’ We gave her penicillin at home. She’s back to gardening. This isn’t science fiction. It’s basic medicine. Stop letting outdated labels kill people. Test. Educate. Update. It’s not hard. It’s just neglected. And that’s on us.