Methadone and QT Prolongation: Essential ECG Monitoring Guidelines
 Nov, 21 2025
Nov, 21 2025
Methadone QTc Calculator
Corrected QT Interval (QTc)
Risk Assessment
Clinical Guidance
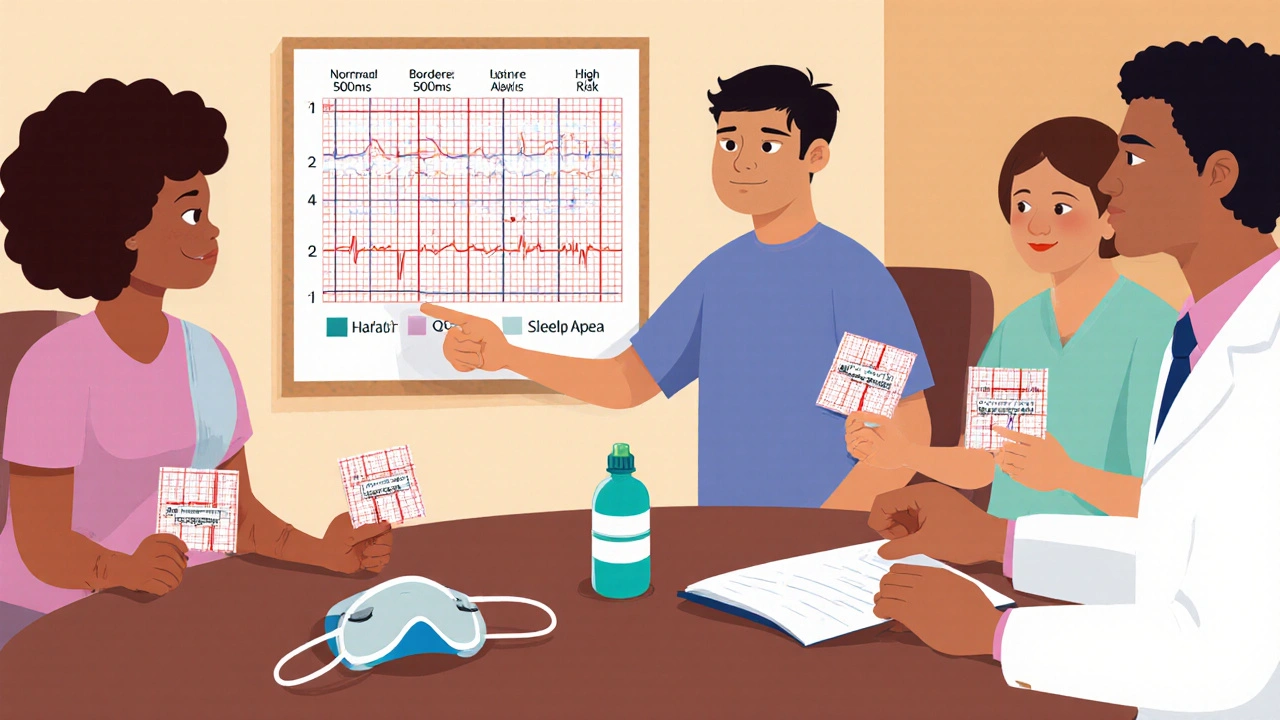
Based on FDA guidelines, QTc >500 ms requires immediate action. Consider dose reduction, electrolyte correction, or alternative therapy. For QTc >500 ms, risk of Torsades de Pointes quadruples.
When someone starts methadone for opioid dependence, the focus is often on reducing cravings and keeping them off street drugs. But there’s a silent risk hiding in plain sight: methadone can stretch the heart’s electrical cycle, leading to a dangerous condition called QT prolongation. Left unchecked, this can trigger a life-threatening arrhythmia called Torsades de Pointes - and in some cases, sudden death. The good news? This risk is predictable, measurable, and preventable with the right ECG monitoring.
Why Methadone Affects Your Heart
Methadone doesn’t just act on opioid receptors in the brain. It also blocks a specific potassium channel in heart muscle cells called hERG (KCNH2). This channel helps the heart reset after each beat. When it’s blocked, the heart takes longer to recharge - and that delay shows up on an ECG as a longer QT interval. The longer the QT interval, the higher the chance of an irregular heartbeat. This isn’t theoretical. Since the FDA issued a safety alert in 2006, over 140 confirmed cases of Torsades de Pointes linked to methadone have been reported - and experts believe many more go unrecorded because sudden deaths in this population are often labeled as overdoses.What’s a Normal QT Interval?
Not all QT prolongation is the same. Doctors measure the corrected QT interval (QTc) to account for heart rate. Here’s what matters:- Normal: ≤430 ms for men, ≤450 ms for women
- Borderline: 431-450 ms (men), 451-470 ms (women)
- Significant prolongation: >450 ms (men), >470 ms (women)
- High risk: >500 ms - this quadruples the risk of sudden cardiac death
A QTc above 500 ms is a red flag. Even a jump of 60 ms from baseline should trigger action. The risk isn’t linear - it spikes sharply past 500 ms. That’s why monitoring isn’t optional. It’s life-saving.
Who’s at Highest Risk?
Not everyone on methadone needs the same level of monitoring. Risk isn’t just about the dose. It’s about the whole picture. These factors stack up:- Female gender - women have 2.5 times higher risk than men
- Age over 65
- Low potassium (<3.5 mmol/L) or low magnesium (<1.5 mg/dL)
- Heart disease - especially heart failure with ejection fraction below 40%
- Slow heart rate (below 50 bpm)
- History of congenital long QT syndrome
- Taking other QT-prolonging drugs - like certain antidepressants (TCAs), antipsychotics (haloperidol), or antibiotics (moxifloxacin)
Here’s the kicker: many patients on methadone are taking at least two of these risk factors. A 2017 study of 127 patients found that 28% had QTc prolongation. Of those, nearly 9% were above 500 ms. The strongest predictors? Daily methadone doses over 100 mg, low potassium, and using other psychotropic medications.
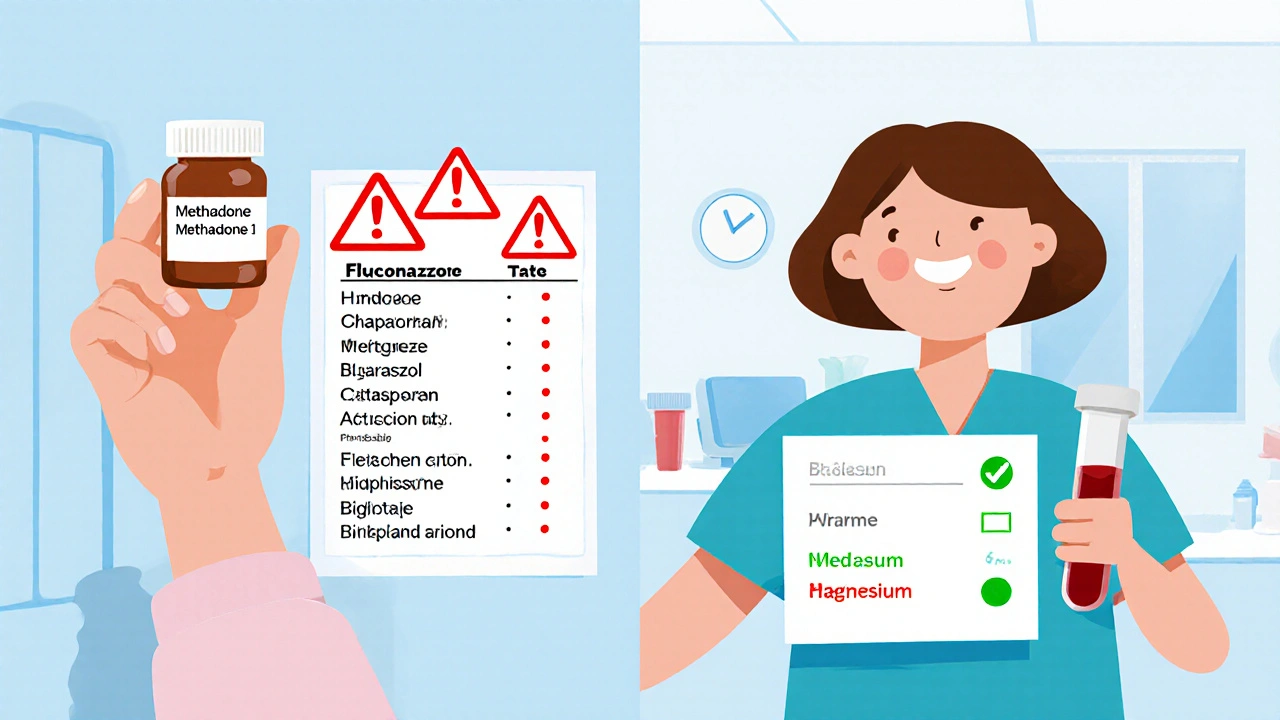
Drug Interactions That Amplify the Danger
Methadone is broken down by the liver using the CYP3A4 enzyme. If something blocks that enzyme, methadone builds up in your blood - and so does the cardiac risk. Common culprits include:- Antifungals: fluconazole, voriconazole
- Some antidepressants: fluvoxamine, citalopram, escitalopram
- Some HIV meds and antibiotics
These aren’t rare drugs. Fluconazole is commonly prescribed for yeast infections. Fluvoxamine is used for anxiety and depression. Many patients don’t realize these can be dangerous when mixed with methadone. Always check new prescriptions with your provider. Even over-the-counter meds like some antihistamines can interfere.
When and How Often to Get an ECG
Guidelines now use a risk-based approach. There’s no need to scan every patient weekly - but you can’t skip it entirely.- Baseline ECG: Required before starting methadone, no exceptions. This sets your personal baseline.
- After dose changes: Wait 2-4 weeks for levels to stabilize, then repeat ECG.
- Low risk: QTc under 450 ms (men) or 470 ms (women), no other risk factors → every 6 months
- Moderate risk: QTc 450-480 ms (men) or 470-500 ms (women), or 1-2 risk factors → every 3 months
- High risk: QTc over 480 ms (men) or 500 ms (women), or 3+ risk factors → monthly ECG, consider lowering dose or switching to buprenorphine
Patients with QTc over 500 ms or a rise of more than 60 ms from baseline should get immediate cardiology input. Electrolytes need checking. Dose reduction is often the next step. Buprenorphine is a safer alternative for many - it carries far less QT risk.
What Happens If You Skip Monitoring?
A 2023 study in JAMA Internal Medicine looked at methadone clinics that implemented structured ECG monitoring versus those that didn’t. The results were clear: clinics with regular ECGs saw a 67% drop in serious cardiac events. That’s not a small benefit. That’s life or death.On Reddit, patients in recovery forums report wide inconsistencies. One user wrote: “I got an ECG when I started, then never again for two years.” Another said: “My clinic does it every month - I sleep better knowing they’re watching my heart.” In a survey of 142 users, 68% said monitoring was inconsistent. But 82% of those who got regular ECGs felt safer - compared to just 47% of those who didn’t.
Other Hidden Risks
Sleep apnea is incredibly common in people on methadone - affecting up to half of patients. When breathing stops during sleep, oxygen drops. That stress on the heart can trigger arrhythmias, especially if the QT interval is already stretched. If you snore loudly, wake up gasping, or feel exhausted during the day, ask for a sleep study. Treating sleep apnea isn’t just about energy - it’s about protecting your heart.What to Do If You’re on Methadone
You don’t need to be scared. You need to be informed. Here’s what to do:- Get a baseline ECG before starting methadone - don’t wait.
- Ask your provider: “What’s my QTc? Is it stable?”
- Keep a list of all your medications - including supplements and OTC drugs - and review it every visit.
- Get blood tests for potassium and magnesium at least once a year, or more if you’re on diuretics or have vomiting/diarrhea.
- Report dizziness, fainting, palpitations, or shortness of breath immediately - even if you think it’s “just stress.”
- If you’re on high doses (>100 mg/day) or have risk factors, insist on regular ECGs - every 3 or 6 months, depending on your level.
There’s no shame in asking for an ECG. This isn’t about distrust - it’s about smart care. Methadone saves lives. But it demands respect for its side effects. Monitoring isn’t bureaucracy. It’s part of the treatment.
What’s Next?
The field is moving toward more proactive care. Some clinics now use automated ECG alerts that flag QTc changes in real time. Others are integrating ECG results directly into electronic health records with built-in risk calculators. These tools aren’t perfect - but they’re helping close the gap between guidelines and real-world practice.If you’re a patient, ask your clinic: “Do you have a formal QT monitoring protocol?” If you’re a provider, don’t assume someone else is watching. Make ECGs part of your standard care - not an afterthought.
Can methadone cause sudden death even if I don’t overdose?
Yes. Methadone can cause a dangerous heart rhythm called Torsades de Pointes, which can lead to sudden cardiac arrest even without drug overdose. This risk is tied to QT prolongation, not the opioid effect. Many deaths in this population are misclassified as overdoses when they’re actually arrhythmias.
Is buprenorphine safer for my heart than methadone?
Yes. Buprenorphine carries significantly less risk of QT prolongation. Studies show it rarely causes clinically meaningful QTc increases, even at high doses. For patients with multiple cardiac risk factors, buprenorphine is often the preferred alternative. Switching isn’t always easy, but it’s medically justified when cardiac safety is a concern.
How often should I get my potassium checked?
At least once a year. If you’re on doses over 100 mg/day, have heart disease, take diuretics, or have had vomiting or diarrhea recently, check every 3-6 months. Low potassium is one of the top modifiable risk factors for methadone-related arrhythmias.
Can I still take antidepressants while on methadone?
Some are safe, others are risky. Avoid citalopram, escitalopram, and fluvoxamine - they can raise methadone levels and prolong QT. Sertraline and bupropion are generally safer choices. Always tell your psychiatrist you’re on methadone before starting any new antidepressant.
What if my clinic won’t do regular ECGs?
You have the right to safe care. Ask for a written policy on QT monitoring. If they don’t have one, request a referral to a cardiologist or a clinic with standardized protocols. Many hospitals and community health centers offer this service. Your recovery shouldn’t come at the cost of your heart health.
Kelsey Worth
November 22, 2025 AT 04:31so like... methadone makes your heart do the cha-cha and no one checks? 😅 i mean, we monitor blood sugar for diabetics but this? we just hand out pills like candy. fix the system, not the symptoms.
shelly roche
November 23, 2025 AT 03:30thank you for putting this out there. i’ve seen too many people get written off as ‘just another overdose’ when it was really their heart giving out. QT monitoring should be standard, not optional. it’s not rocket science - just basic care. let’s stop pretending we’re saving lives while ignoring the most obvious red flags.
Nirmal Jaysval
November 24, 2025 AT 20:50lol u guys act like this is news. i been in india and they dont even have ecg machines in most clinics. here u got all this fancy tech and still people die. its not the drug, its the system. fix that first.
Emily Rose
November 24, 2025 AT 21:59if you’re on methadone, get an ecg before week 2. period. no excuses. this isn’t about being paranoid - it’s about being alive. i’ve had patients flatline because no one checked. don’t be that person. don’t be that provider. check the QT. it takes 3 minutes.
Benedict Dy
November 25, 2025 AT 07:54The data is unequivocal: methadone-induced QT prolongation is a Class I clinical concern. The FDA’s 2006 advisory was not a suggestion - it was a mandate. Failure to adhere to ECG monitoring protocols constitutes a breach of the standard of care and exposes clinicians to significant liability. It is not merely prudent - it is obligatory.
Emily Nesbit
November 26, 2025 AT 16:25QTc >500ms quadruples mortality risk. Yet clinics still prescribe 120mg/day without baseline ecgs. This isn’t negligence. It’s systemic malpractice. Someone needs to sue a few clinics into compliance.
John Power
November 27, 2025 AT 20:22i get it - we’re all busy. but imagine if this was diabetes. would we just hand out insulin and hope for the best? no. we test, we track, we adjust. methadone’s no different. a simple ecg could save someone’s life. it’s not hard. it’s just human.
Richard Elias
November 29, 2025 AT 13:21women are 2.5x more at risk? yeah right. they always overreact. just tell em to stop being weak and take their pills like men. also why are we even talking about this? its not like people on methadone are saints anyway.
Scott McKenzie
November 30, 2025 AT 14:23just got my first methadone script. did the ecg before my first dose. QTc was 412. felt good knowing i’m being cared for. 🙌 if you’re on it - don’t skip the check. it’s the bare minimum. you deserve to live.
Jeremy Mattocks
December 1, 2025 AT 20:24it’s not just about the initial ecg - it’s about serial monitoring. methadone’s half-life is 24 to 36 hours, but its cardiac effects can accumulate over days, especially with dose increases or drug interactions. a single baseline is meaningless if you don’t recheck after dose changes, after adding antibiotics like azithromycin, or after electrolyte imbalances. we’ve seen patients go from 440 to 520 in three days. that’s not a fluke - it’s a predictable cascade. protocols need to reflect that. we need scheduled follow-ups, not just one-and-done screenings. this isn’t theoretical - it’s clinical reality. if your clinic doesn’t have a QT monitoring protocol, demand one. or find a better one.
Paul Baker
December 3, 2025 AT 13:34Zack Harmon
December 4, 2025 AT 00:17THIS IS A MASSACRE. THEY’RE KILLING PEOPLE WITH LEGAL DRUGS AND CALLING IT TREATMENT. SOMEONE’S GOTTA PAY. I’M TALKING HOSPITALS. I’M TALKING DOCTORS. I’M TALKING GOVERNMENT. THIS ISN’T MEDICINE - IT’S A FATAL GAME OF RUSSIAN ROULETTE WITH A HEART.
Jeremy S.
December 5, 2025 AT 19:08check the QT. easy.
Jill Ann Hays
December 5, 2025 AT 20:15The conflation of pharmacokinetic risk with moral worth is a fallacy inherent in contemporary addiction discourse. One cannot ethically justify medical negligence under the guise of harm reduction when the physiological consequences are empirically quantifiable and preventable. The paradigm requires epistemic recalibration.
Mike Rothschild
December 5, 2025 AT 22:40my clinic started doing mandatory ecgs at intake and at 2 weeks. we’ve caught 3 borderline cases so far. two needed dose adjustments. one got a potassium boost. no one died. it’s not hard. it’s just consistent. do the work.
Kelsey Worth
December 7, 2025 AT 18:07and now they’re gonna say ‘but what about the cost?’ like we’re not already spending millions on overdoses and ER visits. one ecg = $80. one death = $1M. math isn’t hard.