Nerve Blocks and RFA: What You Need to Know About Interventional Pain Procedures
 Dec, 19 2025
Dec, 19 2025
Chronic pain doesn’t just hurt-it steals your sleep, your mobility, and your sense of control. If you’ve tried physical therapy, NSAIDs, or even opioids without lasting relief, you might be wondering: is there something more? That’s where nerve blocks and radiofrequency ablation (RFA) come in. These aren’t magic cures, but they’re two of the most reliable, minimally invasive tools doctors use to break the cycle of persistent pain-especially for back, knee, or neck pain that won’t quit.
What Exactly Is a Nerve Block?
A nerve block is a simple injection. A doctor uses imaging guidance-like fluoroscopy or ultrasound-to place a tiny needle right next to a specific nerve that’s sending pain signals. Then, they inject a mix of numbing medicine (like lidocaine) and sometimes a steroid to calm inflammation. The goal? To see if turning off that nerve temporarily makes your pain disappear.If your pain drops by 50% or more after the injection, that’s a strong sign that nerve is the source. Think of it like a diagnostic test. You’re not treating the root cause-like arthritic joints or worn-down discs-but you’re finding out which nerve is screaming the loudest. That’s crucial. Because if you skip this step and jump straight to RFA, you might end up burning the wrong nerve-and get no relief at all.
The relief from a nerve block doesn’t last long. Usually, it’s a few hours to a few weeks. That’s by design. It’s not meant to be a long-term fix. It’s a clue. A signal. A way to say, “Yes, this nerve is the problem.” And if the answer is yes, then RFA becomes the next logical step.
How Radiofrequency Ablation (RFA) Works
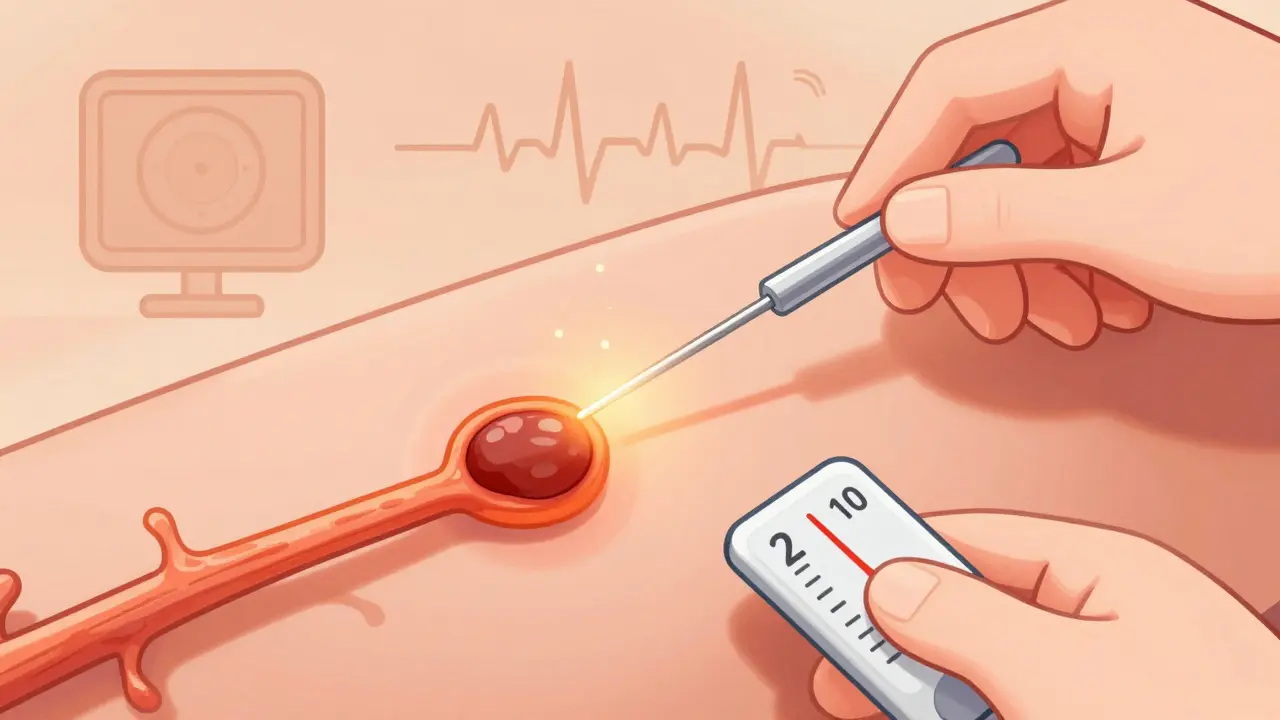
RFA is where things get more permanent. Instead of just numbing the nerve, RFA uses heat to quietly disable it. A thin, insulated needle is guided to the exact same nerve targeted in the diagnostic block. Once it’s in place, a small electric current passes through the tip, creating heat between 80°C and 90°C. That heat creates a tiny lesion-about the size of a pea-on the nerve.This doesn’t destroy the nerve completely. It doesn’t cut it. It doesn’t remove it. It just disrupts its ability to send pain signals. The nerve can regenerate over time, but that takes months. And during that time? You get relief.
The procedure takes 20 to 45 minutes. You’re awake but lightly sedated. You might feel pressure, but you shouldn’t feel sharp pain. The doctor will test the needle’s position before heating it-asking you to report tingling or muscle twitching-to make sure they’re not near a motor nerve. Accuracy matters. A misplaced needle can mean no relief, or even new pain.
Afterward, you might feel sore for a few days. That’s normal. The real pain relief usually starts showing up after two weeks. That’s because the nerve doesn’t stop firing immediately. It takes time for the heat damage to fully block the signal. Most people notice major improvement by the fourth week.
How RFA Compares to Nerve Blocks
| Feature | Nerve Block | Radiofrequency Ablation (RFA) |
|---|---|---|
| Purpose | Diagnostic and short-term relief | Long-term pain control |
| Duration of Relief | Hours to weeks | 6 to 24 months |
| Medication Used | Anesthetic + steroid | Radiofrequency energy (heat) |
| Procedure Time | 10-20 minutes | 20-45 minutes |
| Recovery Time | Same day | 24-48 hours |
| Success Rate (for facet pain) | 30-50% beyond immediate effect | 70-80% in properly selected patients |
| Cost (per procedure) | $500-$1,500 | $3,000-$5,000 |
The big difference? Time. Nerve blocks are like turning off a light switch. RFA is like removing the wiring. One gives you a quick break. The other gives you months of quiet.
And here’s the catch: RFA only works if the nerve block worked first. If your pain didn’t drop significantly after the numbing injection, RFA won’t help. That’s not a failure of the procedure-it’s a failure of selection. About 20-30% of patients who skip the diagnostic step end up disappointed. That’s why every reputable pain clinic insists on it.
Who Benefits Most From RFA?
RFA isn’t for everyone. It’s best for people with chronic pain that’s been stable for at least six months and hasn’t responded to conservative treatments like physical therapy, exercise, or medication.The top candidates:
- People with facet joint pain in the lower back or neck-often from arthritis or degeneration. RFA has a 75% success rate here.
- Those with knee osteoarthritis. Cooled RFA, which treats larger nerves around the knee, helps 65% of patients maintain relief for six months.
- Patients with sacroiliac joint pain. Studies show 70% get meaningful improvement after RFA.
- Anyone who’s tired of taking opioids or NSAIDs long-term.
Age isn’t a barrier. People in their 50s and 60s do best, but even older adults with good overall health can benefit. The key isn’t your age-it’s whether your pain comes from a specific nerve that can be targeted.
What About Pulsed RFA and Cooled RFA?
Not all RFA is the same. There are two main types:- Traditional RFA uses heat to destroy nerve tissue. It’s the standard for facet and SI joint pain.
- Pulsed RFA doesn’t heat the nerve. Instead, it sends short bursts of electrical energy that “reset” the nerve’s pain signals without damaging it. It’s less invasive, with fewer side effects, and is often used for nerve pain like occipital neuralgia or diabetic neuropathy.
- Cooled RFA uses a special probe that circulates cold fluid inside the needle. This lets the heat spread further-creating a larger lesion. That’s why it’s so effective for the knee, where nerves are spread out. Cooled RFA lasts longer than traditional RFA in this area-6 months vs. 3-4 months.
These aren’t new. But they’re getting better. The FDA approved a new pulsed-field system for spinal pain in 2022, and research is now looking at RFA for plantar fasciitis and even chronic headaches. The tools are evolving-and so are the results.
What You Should Know Before Getting RFA
It’s not risky-but it’s not risk-free.- Temporary pain flare: 5-10% of people get nerve inflammation (neuritis) that lasts 1-2 weeks. It feels like a deep ache. Ice and ibuprofen help.
- Inaccurate placement: If the needle isn’t guided perfectly, you might not get relief. That’s why fluoroscopy or ultrasound is non-negotiable.
- Regrowth: Nerves heal. Pain can come back in 6-12 months. That’s normal. Many patients get a second RFA with the same success.
- No cure: RFA doesn’t fix arthritis. It doesn’t rebuild discs. It just blocks the pain signal. You still need to manage your condition with movement, weight control, and physical therapy.
But here’s what most patients say: “I wish I’d done this sooner.”
One woman in her 60s from Dublin, who had chronic lower back pain for 8 years, told her doctor: “I stopped walking to the mailbox because it hurt too much. After RFA, I walked to the park with my grandkids for the first time in years.” That’s the kind of result this procedure delivers-not for everyone, but for enough people to make it a game-changer.

How RFA Fits Into the Bigger Picture
Pain management isn’t about one magic fix. It’s a ladder. At the bottom: rest, exercise, physical therapy. Middle: medications, nerve blocks. Higher up: RFA. At the top: surgery.RFA sits right where most people need it. It’s less invasive than spinal fusion, cheaper than a spinal cord stimulator (which can cost $50,000), and more effective than pills for long-term relief. The American Society of Anesthesiologists recommends it as a second-line treatment after conservative care fails.
And the numbers back it up. In the U.S., over 350,000 RFA procedures are done each year. Medicare data shows patients who get RFA cut their opioid use by 22%. That’s not just pain relief-it’s a public health win.
As technology improves, RFA will likely become even more common. Cooled probes, better imaging, and smarter targeting mean more people will get relief-and for longer.
What Happens After RFA?
You’ll go home the same day. No overnight stay. No catheter. No big bandage.- Day 1: Rest. Don’t drive. Avoid heavy lifting.
- Day 2-3: Start light walking. Gentle stretching.
- Week 1: Resume normal daily activities. Avoid high-impact exercise.
- Week 2-4: Pain relief builds. Keep a pain diary to track progress.
- Month 2: If relief is strong, you can return to most activities. Many patients resume exercise, gardening, even golf.
Most people are back to work within 3 days. Only 5% report complications. And 85% say their pain dropped by half or more.
The key? Stay active. Don’t wait for the pain to vanish completely before moving. Movement helps nerves heal properly. Physical therapy after RFA can double your long-term success.
Are nerve blocks and RFA the same thing?
No. A nerve block uses medicine to temporarily block pain signals. RFA uses heat to disable the nerve for months. Nerve blocks are used to test if RFA will work. You need a successful nerve block before RFA is recommended.
How long does RFA pain relief last?
Most people get relief for 6 to 18 months. Some last up to two years, especially with cooled RFA for knee pain. Nerves eventually regrow, so pain can return. A second RFA is often just as effective as the first.
Is RFA safe?
Yes, when done correctly. Complications are rare-less than 5%. Risks include temporary soreness, nerve irritation, or inaccurate needle placement. Using imaging guidance and following diagnostic criteria reduces these risks significantly.
Can RFA help with knee pain from arthritis?
Yes. Cooled RFA targets the genicular nerves around the knee. Studies show 65% of patients get at least 50% pain relief for six months. That’s better than cortisone shots, which often wear off in 3 months.
Do I need to stop my medications before RFA?
You’ll usually be asked to stop blood thinners like warfarin or aspirin 5-7 days before. NSAIDs can be continued unless your doctor says otherwise. Always follow your provider’s instructions-never stop meds on your own.
What if RFA doesn’t work?
If you didn’t get relief, it’s likely because the diagnostic nerve block didn’t accurately identify the pain source. Other causes-like disc problems, muscle strain, or referred pain-might be responsible. Further testing or a different treatment may be needed.
Is RFA covered by insurance?
Most insurance plans, including Medicare and private insurers, cover RFA when it follows a successful diagnostic nerve block and is for approved conditions like facet joint pain or knee osteoarthritis. Pre-authorization is usually required.
Next Steps: Is RFA Right for You?
If you’ve been living with chronic pain for over six months and nothing else has given you lasting relief, talk to a pain specialist. Ask if you’re a candidate for a diagnostic nerve block. If it works, RFA could be your next step.This isn’t about avoiding surgery. It’s about avoiding unnecessary suffering. You don’t have to live with pain that keeps you from walking, sleeping, or playing with your kids. RFA doesn’t promise perfection-but for many, it promises peace. And that’s worth more than most people realize.
Janelle Moore
December 19, 2025 AT 14:52Erica Vest
December 19, 2025 AT 22:28Chris Davidson
December 20, 2025 AT 19:37Glen Arreglo
December 21, 2025 AT 06:56Ashley Bliss
December 22, 2025 AT 23:16Allison Pannabekcer
December 23, 2025 AT 20:34Sarah McQuillan
December 24, 2025 AT 08:39Mark Able
December 25, 2025 AT 17:47Kevin Motta Top
December 26, 2025 AT 10:49Henry Marcus
December 27, 2025 AT 15:22