Opioid Reactions: How to Tell Itching from a Real Allergy and What to Do
 Nov, 25 2025
Nov, 25 2025
Many people who take opioids for pain end up with itchy skin. It’s common. So common, in fact, that most patients assume it’s an allergy. But here’s the truth: itching from opioids is rarely a true allergy. In fact, up to 80% of what people call an "opioid allergy" is actually a pseudoallergic reaction - a side effect, not an immune response. And mistaking one for the other can mean you’re denied effective pain relief, forced onto more expensive drugs, or even left in unnecessary discomfort.
Itching Isn’t an Allergy - Here’s Why
When you take morphine or codeine, your body doesn’t always react the way you’d expect. Instead of your immune system attacking the drug, certain cells in your skin - called mast cells - get triggered directly. They dump histamine into your bloodstream. That’s what causes the itch, the flushing, the sneezing, or even mild sweating. It’s not dangerous. It’s not an allergy. It’s just a side effect. This isn’t new science. Researchers figured this out in the 1980s. But the mistake still happens every day. A 2022 study from the University of Michigan looked at over 1,200 patients who said they were allergic to opioids. Eighty-seven percent of them described only itching, nausea, or dizziness. None of those are signs of a true allergic reaction. True opioid allergies are rare. They affect less than 0.3% of people who take opioids. When they do happen, they’re serious: hives, swelling of the throat, trouble breathing, or a sudden drop in blood pressure. These reactions happen fast - within minutes - and involve more than one system in your body. Itching alone? That’s not it.Which Opioids Cause More Itching?
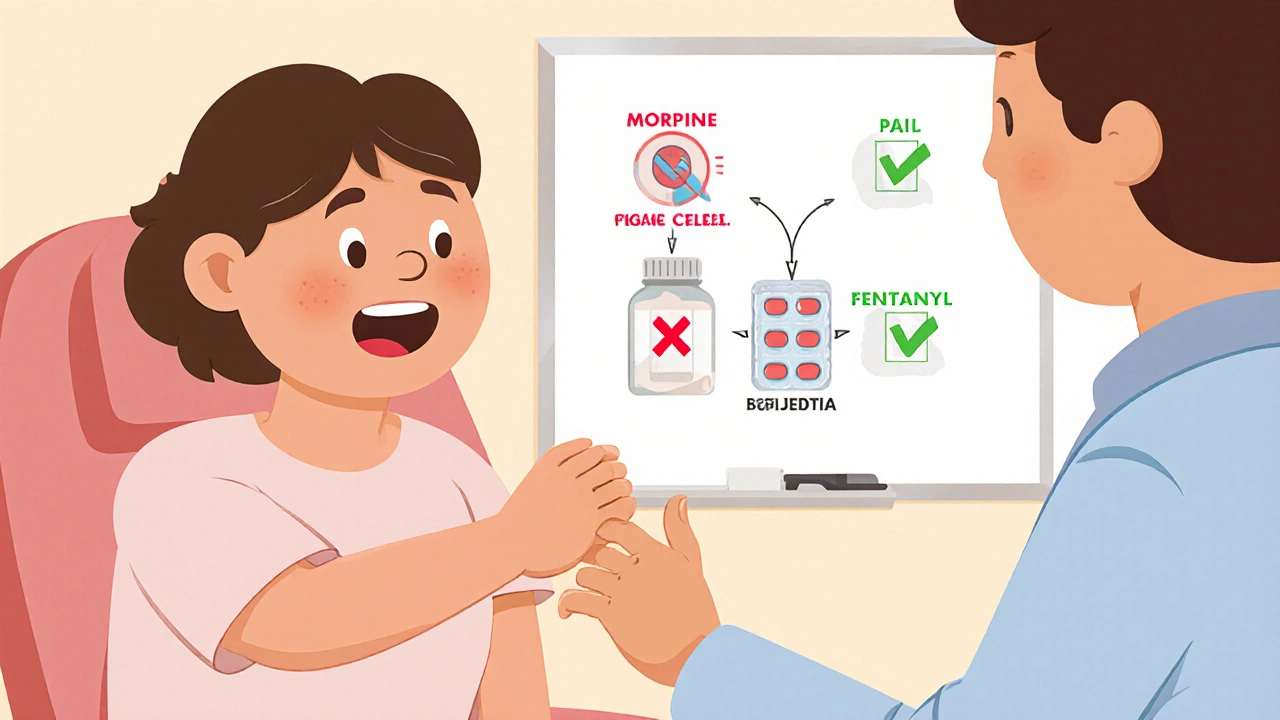
Not all opioids are the same when it comes to itching. Morphine and codeine are the worst offenders. They’re natural opioids with a chemical structure that easily triggers mast cells. Studies show morphine can cause itching in 30-40% of patients. Codeine isn’t far behind. On the other side, synthetic opioids like fentanyl, methadone, and hydromorphone are much less likely to cause itching. Fentanyl, for example, releases 3-4 times less histamine than morphine per milligram. Methadone? Only 5-10% of users report itching. That’s because their chemical makeup doesn’t stimulate mast cells the same way. This matters because if you’ve been told you’re allergic to opioids because you got itchy on morphine, you don’t have to avoid all of them. You might tolerate fentanyl or methadone just fine - especially if you take an antihistamine first.What to Do When You Get Itchy
If you start itching after taking an opioid, don’t panic. Don’t assume you’re allergic. Talk to your doctor. Here’s what works:- Reduce the dose by 25-50%. Often, lowering the amount stops the itching without losing pain control.
- Take an H1 antihistamine like diphenhydramine (Benadryl) 25-50 mg about 30 minutes before your next dose. This helps in 80-90% of cases.
- If itching persists, switch to a different opioid. Fentanyl patches or methadone are good alternatives with lower histamine risk.
Some patients even report that switching from morphine to a fentanyl patch makes all the difference. One Reddit user wrote: "I was labeled allergic to all opioids because I got itchy on morphine. Fentanyl patch works fine with Benadryl." That’s not rare. It’s common.

When It’s Actually an Allergy
True opioid allergies are rare, but they’re real. If you’ve ever had:- Sudden swelling of the lips, tongue, or throat
- Wheezing or trouble breathing
- A drop in blood pressure that made you feel faint or pass out
- A rash that spread quickly and looked like hives or blisters
- then you might have a true allergy. These reactions need immediate medical attention. Epinephrine is the first-line treatment. Avoid that opioid forever. And be cautious with other opioids in the same class - like oxycodone or hydrocodone - since they’re chemically similar to morphine.
But here’s the key: if you only had itching, nausea, or dizziness, you likely don’t have a true allergy. Don’t let a label from years ago stop you from getting proper pain relief now.
What Doctors Are Doing Differently Now
Hospitals and clinics are waking up to this problem. The American Academy of Allergy, Asthma & Immunology updated its guidelines in 2022 to say: don’t label someone allergic to opioids just because they got itchy. Instead, test them properly. Some centers use a simple tool called the Opioid Allergy Assessment Tool. It asks: Did the itching happen right after the dose? Did it get worse with higher doses? Did antihistamines help? Answer those questions correctly, and doctors can identify pseudoallergies 92% of the time. In 2021, Epic Systems - the biggest electronic health record provider - added alerts that separate "itching" from "allergy" in patient charts. Hospitals using it saw a 45% drop in incorrect allergy labels. Even the FDA now requires opioid labels to clearly state that itching is a common side effect, not an allergy. That’s a big shift.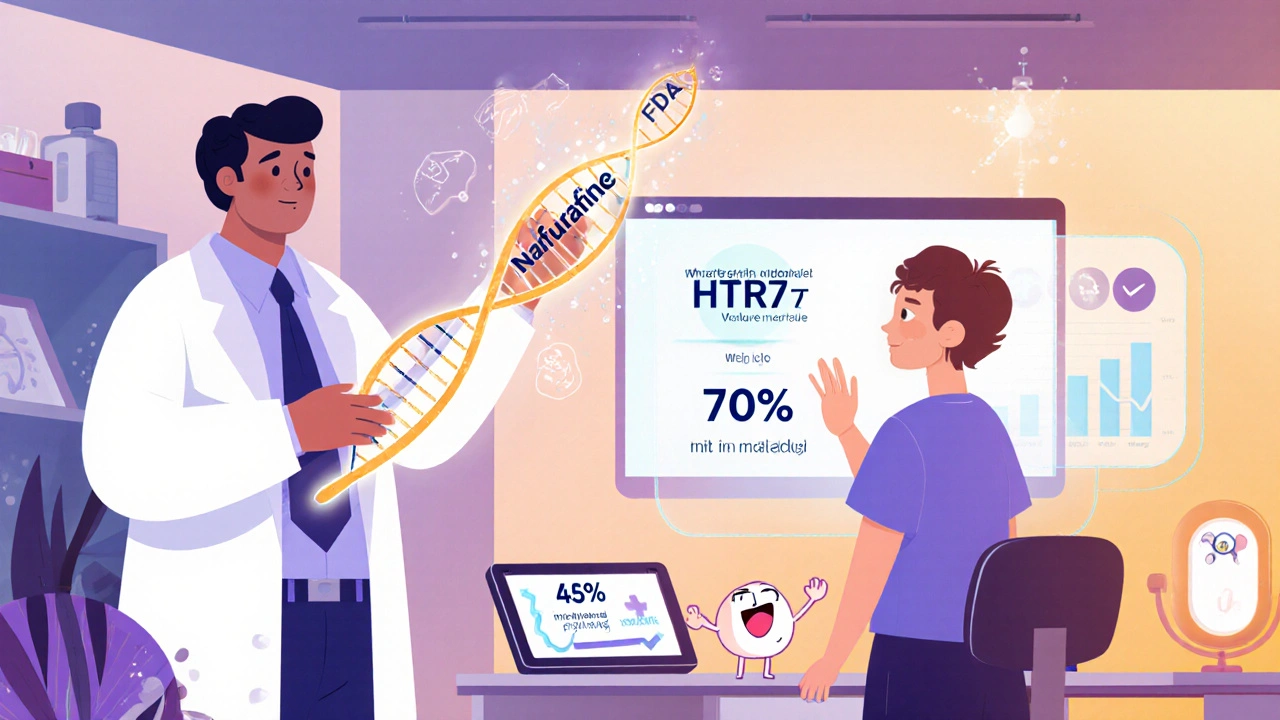
What’s Next? New Treatments on the Horizon
Science is catching up. In 2023, a study in Nature Neuroscience showed that a drug called nalfurafine - already approved in Japan - cuts opioid-induced itching by 70% without reducing pain relief. It’s in late-stage trials in the U.S. and could be available soon. Researchers are also looking at genetic markers. Some people have a version of the HTR7 gene that makes them more likely to release histamine when they take opioids. In the future, a simple blood test might tell you if you’re at higher risk for itching - before you even take the drug. And there’s new hope for pain meds that don’t cause itching at all. Two drugs in development - CR845 and NOP receptor agonists - have shown 80% less itching in trials. They could change the game for chronic pain patients.What You Should Do Today
If you’ve been told you’re allergic to opioids because you got itchy:- Don’t assume you can’t take any opioids again.
- Write down exactly what happened: Was it just itching? Did it happen every time? Did antihistamines help?
- Ask your doctor: "Could this be a pseudoallergy? Can we try a different opioid with antihistamine premedication?"
- If you’ve had swelling, breathing trouble, or low blood pressure - get tested by an allergist. That’s different.
Most people don’t need to avoid opioids forever. They just need the right one - and maybe a little help with an antihistamine.
The bottom line? Itching doesn’t mean you’re allergic. It means you need a better plan. And that plan exists.
Is itching from opioids a sign of a true allergy?
No, itching alone is not a sign of a true opioid allergy. In 70-80% of cases, it’s a pseudoallergic reaction caused by histamine release from mast cells, not an immune response. True allergies involve swelling, trouble breathing, or low blood pressure - not just itching.
Which opioids cause the most itching?
Morphine and codeine cause the most itching, affecting 30-40% of users. Synthetic opioids like fentanyl, methadone, and hydromorphone release far less histamine and cause itching in only 5-15% of people.
Can I still take opioids if I get itchy?
Yes. Most people who get itchy on morphine can tolerate fentanyl or methadone, especially when taking an antihistamine like diphenhydramine before the dose. Reducing the opioid dose by 25-50% also helps in most cases.
Should I get tested for an opioid allergy?
Only if you’ve had severe symptoms like swelling, trouble breathing, or low blood pressure. Skin testing for opioid allergies is unreliable and often gives false positives. For itching alone, a therapeutic trial with a different opioid is safer and more accurate.
What’s the best way to manage opioid-induced itching?
Start by lowering the opioid dose by 25-50%. Then take diphenhydramine (25-50 mg) 30 minutes before the next dose. If itching continues, switch to fentanyl or methadone. These opioids have much lower histamine-releasing potential.
Are there new drugs that don’t cause itching?
Yes. Nalfurafine, approved in Japan, reduces opioid-induced itching by 70% without affecting pain relief. Two new drugs - CR845 and NOP receptor agonists - are in late-stage U.S. trials and show 80% less itching. They’re expected to be available within the next few years.
Why do some doctors still say I’m allergic to all opioids?
Many doctors were trained to assume itching equals allergy. But guidelines updated in 2022 by the American Academy of Allergy, Asthma & Immunology now say that’s wrong. Mislabeling is common - up to 87% of patients labeled "allergic" only had side effects. Ask your doctor to review the latest evidence.
Can I take antihistamines long-term with opioids?
Diphenhydramine is safe for short-term use before opioid doses. But long-term use can cause drowsiness, dry mouth, and confusion - especially in older adults. For ongoing itching, switching to a low-histamine opioid like methadone or fentanyl is a better long-term solution.
Stephanie Deschenes
November 25, 2025 AT 23:42I’ve seen this so many times in my nursing practice. Patients get labeled "allergic" after one itchy episode and then get stuck with NSAIDs that don’t touch their pain. I always suggest trying fentanyl patches with a little Benadryl first-works like magic for most. No need to suffer needlessly.
Also, don’t forget: if they’ve never had swelling or breathing issues, it’s almost certainly not a true allergy. Just a histamine hiccup.
Cynthia Boen
November 26, 2025 AT 05:40Of course the medical system still gets this wrong. It’s easier to say "allergy" than to think. I’ve had to fight for 3 years just to get a decent pain med because some intern wrote "opioid allergy" in my chart after I got itchy on morphine. No one ever asked if antihistamines helped. No one cared. Just write it off and move on.
Douglas Fisher
November 26, 2025 AT 11:45Thank you for this. Honestly, I’ve been terrified to take anything stronger than Tylenol for years because I got itchy on hydrocodone back in 2015. I didn’t know the difference between a pseudoallergy and a real one. This is life-changing information.
I’m going to talk to my pain specialist next week and ask about methadone. I’ve heard it’s less itchy, and now I have actual science to back up asking for it. I feel like I’ve been gaslit by my own medical records.
Amanda Meyer
November 28, 2025 AT 00:03This is an excellent, evidence-based breakdown. The fact that Epic Systems now separates "itching" from "allergy" in EHRs is a monumental step forward. Too many patients are denied appropriate care due to outdated, lazy labeling.
I also appreciate the emphasis on therapeutic trials over unreliable skin testing. Allergists should be consulted only for true anaphylactic reactions-not for histamine-mediated side effects.
Let’s hope this becomes standard training in med school. We’re still seeing this mistake in residency programs.
Jesús Vásquez pino
November 29, 2025 AT 09:03Wait, so you’re telling me I don’t have to avoid all opioids just because I got itchy on morphine? That’s it? No more "you’re allergic to everything"? I’ve been on gabapentin for 5 years because no one would touch me with a 10-foot pole. I’m crying right now. This is the first time anyone’s ever validated me.
Can someone send me a link to the FDA’s new labeling requirement? I’m printing this out and handing it to my doctor tomorrow.
hannah mitchell
November 30, 2025 AT 23:33I got itchy on codeine after surgery. Took Benadryl next time, no problem. Still take it when I need it. Never had a real allergic reaction. Just weird how everyone assumes the worst. My doctor just shrugged and said "allergy" and moved on. Glad someone’s finally explaining it properly.
vikas kumar
December 2, 2025 AT 05:29As someone from India where opioids are still stigmatized and rarely prescribed, I find this incredibly useful. Even here, patients panic at the first sign of itching and refuse meds. This kind of education could save so many from chronic pain.
Maybe we need a simplified version in Hindi or Urdu? I’d love to translate this for my community. The confusion here is even worse.
Vanessa Carpenter
December 2, 2025 AT 19:40My mom had chronic back pain and was told she was allergic to everything because she got itchy on oxycodone. She ended up on tramadol for years-worked okay, but made her feel foggy. Last year we tried fentanyl patch with diphenhydramine. She hasn’t looked back. I’m so glad this info is out there. She deserves better.
Bea Rose
December 3, 2025 AT 17:1980% pseudoallergy? That’s not a statistic. That’s a systemic failure. You’re telling me doctors have been mislabeling patients for decades because they didn’t read the 1980s literature? And now it’s a "big shift" because Epic added a checkbox? We’re still playing catch-up because nobody cared enough to update training.
Stop calling it progress. Call it damage control.
Michael Collier
December 5, 2025 AT 06:29It is with profound gratitude that I acknowledge the thoroughness and clinical precision of this exposition. The integration of peer-reviewed data, institutional policy updates, and pharmacological mechanisms provides a paradigmatic model for patient education in the context of adverse drug reactions.
It is imperative that healthcare institutions disseminate this knowledge through mandatory continuing education modules, particularly in emergency medicine and palliative care domains.
Furthermore, the adoption of standardized assessment tools, such as the Opioid Allergy Assessment Tool, should be codified into institutional protocols to mitigate diagnostic error and promote equitable access to analgesia.
Shannon Amos
December 6, 2025 AT 10:16So let me get this straight… I’ve been avoiding pain meds for 10 years because I got itchy… and the solution was to take Benadryl the whole time? Classic. I’m basically a walking medical meme.
Thanks for the laugh and the life-changing info. I’m gonna go ask my doctor if I can finally stop being a martyr for bad medical records.
Ryan C
December 6, 2025 AT 19:00Correction: The 2022 University of Michigan study reviewed 1,247 patients-not "over 1,200." Also, nalfurafine is a kappa-opioid receptor agonist, not a "new drug"-it’s been used in Japan since 2009. And CR845 is now called difelikefalin, which was FDA-approved in 2021 for pruritus in CKD-not yet for opioid-induced itching. Please fact-check before posting. 🙄
Also, diphenhydramine is an H1 blocker, not an "antihistamine" in the general sense-there are H2 blockers too. Precision matters.
Dan Rua
December 8, 2025 AT 00:33This is the kind of post that makes me feel less alone. I’ve been scared to even mention opioids to my doctor for years. Now I know I’m not allergic-I just need the right one. I’m going to try methadone with Benadryl next week. Fingers crossed.
Thank you for sharing this. You saved me from years of unnecessary suffering. 🙏
Stephanie Deschenes
December 9, 2025 AT 18:26One thing to add: if you’re on long-term opioids and itching persists even with antihistamines, consider switching to hydromorphone. It’s not as widely known, but it’s one of the lowest histamine-releasing opioids out there-often better than fentanyl for chronic use. And it’s not as sedating as methadone.
Also, don’t forget: itching can get worse with repeated dosing. That’s why lowering the dose helps. It’s not tolerance-it’s histamine buildup.