Patient Assistance Programs from Drug Companies: Eligibility Criteria Explained
 Dec, 5 2025
Dec, 5 2025
Getting the medicine you need shouldn’t mean choosing between rent and refills. For millions of Americans, patient assistance programs from drug companies are the only way to afford life-saving prescriptions. But qualifying isn’t simple. Income limits, insurance status, and paperwork requirements vary wildly between companies - and one wrong detail can get your application denied.
Who Qualifies for Patient Assistance Programs?
Most programs target people who can’t afford their meds, but the rules aren’t the same everywhere. The biggest factor? Income. Nearly all programs use the Federal Poverty Level (FPL) as their baseline. For 2023, 500% of FPL meant $75,000 a year for a single person and $153,000 for a family of four. Some programs, especially for expensive cancer or rare disease drugs, go as high as 600% FPL. Others, like those for common conditions like diabetes or high blood pressure, cap eligibility at 300% or 400% FPL.Here’s how it breaks down by company:
- Pfizer’s RxPathways: 300% FPL ($43,200 single) for primary care drugs like Eucrisa; up to 600% FPL ($77,760 single) for specialty and oncology meds.
- GSK’s Patient Assistance Foundation: $58,650 yearly for one person; $120,570 for a family of four.
- Merck: Generally requires being uninsured, but allows insured patients with documented financial hardship.
- AbbVie: Eligibility depends on the specific drug you’re prescribed - you pick your medicine first, then check if you qualify.
It’s not just about gross income. Most programs require Modified Adjusted Gross Income (MAGI), which includes wages, Social Security, unemployment, and even child support. Many applicants mess up by using gross income instead - a mistake that causes 31% of initial denials, according to internal data from major pharmaceutical firms.
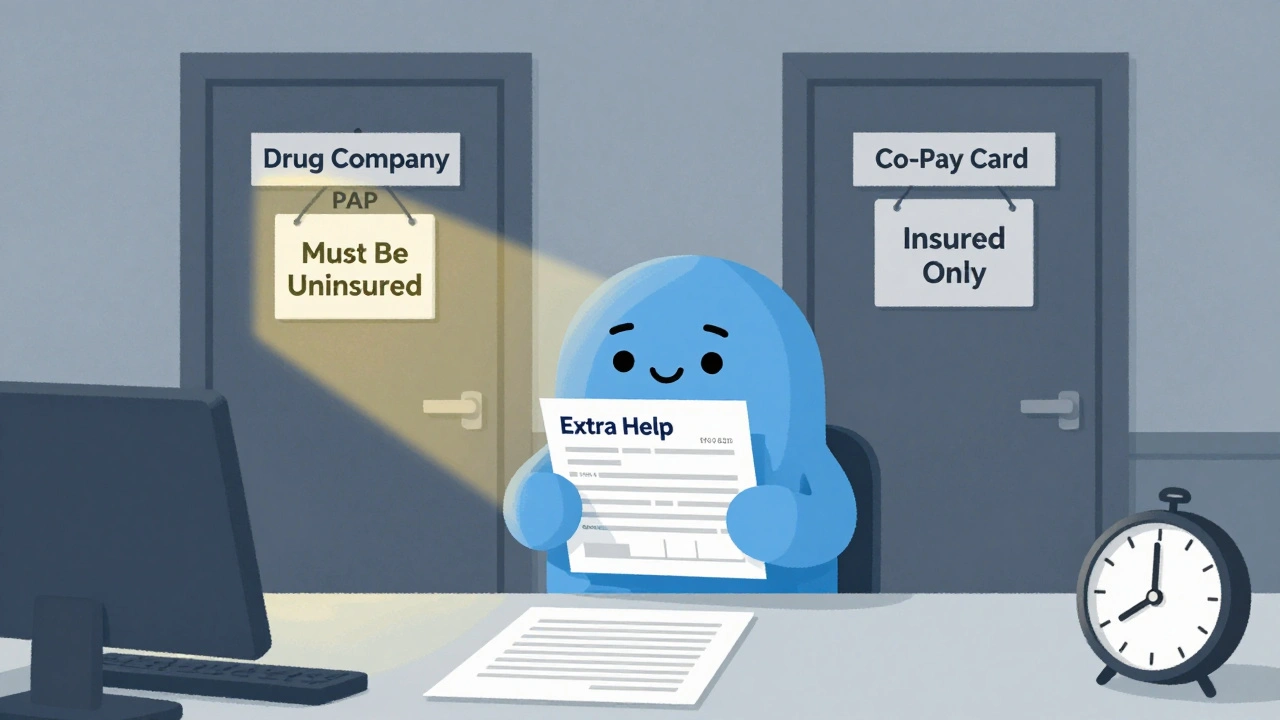
Insurance Status: The Biggest Trap
This is where most people get stuck. You’d think if you have insurance, you’re covered. But for many PAPs, having insurance means you’re automatically disqualified.Here’s the twist: 97% of independent charity PAPs (like PAN Foundation or HealthWell) won’t help you if you’re uninsured. That’s right - the very people who need help the most are often turned away. Meanwhile, manufacturer programs like Pfizer’s Patient Assistance Program require you to be uninsured or underinsured by government plans. If you have private insurance, you’re out.
Medicare beneficiaries face an even trickier situation. If you’re on Medicare Part D, you might be eligible for Extra Help - a federal program that lowers your drug costs. But if your income is between 135% and 150% FPL (about $18,347-$20,385 for one person), you don’t qualify for Extra Help… and most drug company PAPs won’t help you either. That’s the “Medicare gap” - a real hole in the safety net.
Takeda’s Help At Hand program requires Medicare patients to apply for Extra Help first. If they’re denied, then - and only then - can they apply for Takeda’s assistance. You need to submit the denial letter. No letter? No help.
Residency and Treatment Requirements
You must live in the U.S. and be treated by a doctor licensed here. That’s non-negotiable. All major programs - Pfizer, Merck, AbbVie, GSK - require proof of U.S. address. That means a utility bill, lease agreement, or government mail with your name and current address. No exceptions.Your prescriber must also be a U.S.-licensed physician. If you’re seeing a doctor overseas or even a telehealth provider not licensed in your state, you won’t qualify. Even if you’re a U.S. citizen living abroad, you’re out of luck.
What Documents Do You Need?
The paperwork is heavy. Most programs require:- Completed application form (signed by you and your doctor)
- Proof of income: W-2s, recent pay stubs, tax returns, or Social Security award letters
- Proof of identity: Driver’s license, state ID, or passport
- Proof of U.S. residency: Utility bill, bank statement, or lease
- Prescription for the specific drug you need
- Physician verification form (often separate from the prescription)
Doctors are required to sign off - and that’s where delays happen. Merck reports it takes an average of 28 days to get a doctor’s form back. If your doctor’s office is slow, your approval gets pushed back. Some programs now let you upload documents online, but others still require mailed originals.
One of the most common mistakes? Getting household size wrong. If you’re applying as a single person but live with a partner or adult child who contributes to household income, you must include them. CMS analysis in 2022 found 52% of errors came from incorrect household size calculations.
What If You’re Denied?
Denials happen - often. Reddit users on r/medicare report a 37% initial denial rate. The top reasons? Missing documents (68%) and income verification issues (22%).Don’t give up. Most programs let you reapply. The Medicare Rights Center found 42% of people needed three or more tries to get approved. Here’s what to do:
- Check the denial letter - it should say exactly why you were turned down.
- Fix the issue: If it’s income documentation, get updated pay stubs or a letter from your employer.
- Call the program’s patient support line. Many have navigators who can walk you through the process.
- Ask your doctor to re-sign forms or write a letter explaining your medical need.
Some programs, like Pfizer’s RxPathways, now link directly to TurboTax to auto-fill income data - cutting application errors by nearly a third. If your program offers electronic verification, use it.
How Long Does Approval Take?
Once everything’s in, approval can be fast - or slow. If your application is complete and accurate, you could get your meds within 72 hours. That’s what 89% of CMS beneficiaries reported.But if something’s missing? You’re looking at 2-6 weeks. AbbVie’s own user testing found the average application takes 27.3 minutes to fill out. That’s not long - but if you’re juggling jobs, childcare, or health appointments, it’s hard to get right the first time.
Do You Have to Reapply?
Yes. Most programs require re-enrollment. For common medications like insulin or blood pressure pills, you’ll need to re-verify once a year. For specialty drugs - cancer treatments, rare disease meds - you might need to reapply every 3 to 6 months.GSK requires annual re-enrollment. Pfizer’s specialty drug programs ask for updated income proof every quarter. If you miss the deadline, your meds stop. No warning. No grace period.

What About Medicare Part D?
This is critical. If you’re on Medicare Part D, assistance from manufacturer PAPs does not count toward your True Out-of-Pocket (TrOOP) costs. That means even if a drug company gives you $10,000 worth of free medicine, it won’t help you reach the $8,000 TrOOP threshold needed to get catastrophic coverage in 2024.That’s a major flaw. You’re getting free drugs - but still stuck paying high costs later. CMS has been clear: PAPs must stay separate from Part D calculations. This is why some experts call these programs a band-aid, not a fix.
Are These Programs Getting Easier?
A little. In 2023, 12 major drug companies launched “commercial PAPs” - programs for people with private insurance who still face high copays. These are new, and they’re growing fast.Pfizer, Merck, and AbbVie now offer co-pay cards that reduce your monthly cost to $0 or $10. These aren’t the same as PAPs - they’re for insured patients. But they’re helping more people than ever before.
Also, tools like the Medicine Assistance Tool (MAT) let you search multiple programs at once. It’s not perfect, but it’s better than calling 10 different companies.
Still, the system is broken. Drug companies spent $32.7 billion on PAPs in 2022 - but the U.S. spent $600 billion on prescriptions. That’s 5.5% of total spending. Critics say this lets companies keep prices sky-high while looking like they care. The Inflation Reduction Act’s $2,000 out-of-pocket cap for Medicare Part D in 2025 will likely reduce PAP use by 35-40%. That’s good for patients - but it also means these programs may shrink.
Where to Start
If you need help:- Find your drug’s manufacturer website. Search “[Drug Name] patient assistance program.”
- Use the Medicine Assistance Tool (MAT) at medicationassistancetool.org (you can search by drug, income, insurance).
- Call your pharmacy - many have patient advocates who know which programs accept your insurance.
- Ask your doctor’s office if they have a patient support coordinator.
Don’t wait until you run out. Start early. Get your documents ready. And don’t take ‘no’ for an answer - reapply. Thousands get approved on their second or third try.
Can I get free medicine if I have Medicare?
Yes, but only under specific conditions. Most drug company PAPs require you to be uninsured or underinsured by government programs. If you’re on Medicare Part D, you may qualify only if you’ve been denied Extra Help and your income is below 150% of the Federal Poverty Level. Some manufacturers offer separate co-pay assistance for Medicare patients - check their websites directly.
Do I need to be completely uninsured to qualify?
No - but it depends on the program. Manufacturer PAPs like Pfizer’s require you to be uninsured or underinsured by government plans. Independent charities often exclude the uninsured entirely. Some newer programs, called commercial PAPs, help people with private insurance who have high out-of-pocket costs. Always check the specific program’s rules.
What if my income is just above the limit?
You might still qualify if you have high medical expenses. Some programs allow deductions for out-of-pocket health costs, childcare, or disability-related expenses when calculating income. Others have hardship exceptions. Call the program directly - don’t assume you’re ineligible. Many applicants are turned down for reasons that can be appealed.
How long does the approval process take?
If your application is complete and accurate, you can get approved in as little as 72 hours. But if documents are missing or income verification is unclear, it can take 2-6 weeks. The biggest delays come from waiting for your doctor to sign forms. Start early and follow up with your provider.
Do I have to reapply every year?
Yes, most programs require annual re-enrollment. For expensive specialty drugs, you may need to reapply every 3-6 months. You’ll need to submit updated income documents and proof of continued medical need. Missing a deadline means your medication will stop - no warning.
Can I use PAPs and a co-pay card together?
No. If you’re enrolled in a manufacturer’s patient assistance program, you can’t also use their co-pay card. Co-pay cards are for insured patients. PAPs are for those without coverage or with limited coverage. Using both violates program rules and can result in termination.
What if I don’t have a tax return?
You can still qualify. If you didn’t file taxes, you can submit W-2s, pay stubs, unemployment statements, or a signed letter from your employer stating your income. Some programs accept a signed affidavit of income if other documents aren’t available. Call the program to ask what alternatives they accept.
Are there programs for children or seniors?
Yes. Most programs don’t restrict by age - eligibility is based on income and insurance status. Seniors on Medicare can qualify for certain programs if they meet income limits and have been denied Extra Help. Children qualify under their household’s income, regardless of age. Some programs even offer free medications for pediatric conditions like asthma or epilepsy.
joanne humphreys
December 6, 2025 AT 04:59I applied for Pfizer's program last year for my insulin. Got denied because they counted my boyfriend's income even though he doesn't live with me. Took three calls and a notarized letter from my landlord to fix it. Don't assume you're out - push back.
Doctors are the real bottleneck. Mine took 3 weeks to sign the form. I had to go in person and bribe them with coffee.
Priya Ranjan
December 7, 2025 AT 22:10If you can't afford medicine, why are you living in America? Other countries have universal healthcare. This whole system is a joke. You're being exploited by pharma giants and your own government.
Stop begging for scraps. Demand change. This isn't charity - it's a human right.
Gwyneth Agnes
December 9, 2025 AT 19:32Denied twice. Got it on third try. Documents matter. Income math matters. Don't guess. Do it right.
Kay Jolie
December 11, 2025 AT 16:36Let’s be real - this isn’t assistance, it’s performative philanthropy. These companies spend $32B on PAPs while charging $1,200 for a vial of insulin that costs $2 to produce. They’re using these programs as PR armor while lobbying Congress to block price caps.
The real solution? Single-payer. Or at least, force them to cap prices at manufacturing cost + 10%. But no - we’d rather let patients play paperwork roulette while executives take bonuses.
And don’t get me started on the Medicare TrOOP loophole. That’s not a bug - it’s a feature designed to keep you trapped in the system. Brilliant, really. If you’re not furious, you’re not paying attention.
pallavi khushwani
December 12, 2025 AT 14:41I’ve been helping friends navigate these programs for years. It’s heartbreaking how many people give up after one denial. The system isn’t broken - it’s designed to exhaust you.
But here’s the thing: if you have someone who can sit with you, help you fill forms, call the support line - you have a shot. I’ve seen people get approved after 5 tries. One woman got her cancer drug after her neighbor drove her to the post office every week to mail docs.
We need community networks. Not just corporate charity.
Dan Cole
December 13, 2025 AT 21:50Let’s analyze the structural flaw: 97% of independent charity PAPs exclude the uninsured, yet the uninsured are the most vulnerable demographic. This is not a gap - it’s a deliberate misalignment of incentives. Charities are funded by donors who prefer to help the ‘deserving’ - i.e., those with insurance but high copays. The truly destitute are collateral damage.
Furthermore, the MAGI requirement is archaic. It ignores regional cost-of-living disparities. A $50k income in rural Mississippi is not equivalent to $50k in San Francisco. Yet the FPL is national. This is not policy - it’s bureaucratic laziness dressed as equity.
Billy Schimmel
December 14, 2025 AT 02:35My aunt got her blood pressure med for free for 3 years. Then they stopped sending it. No email. No call. Just silence.
She had to start skipping doses. Now she’s in the hospital.
So yeah. Good luck.
Max Manoles
December 15, 2025 AT 20:54One thing the article doesn’t mention: many programs require you to reapply every quarter for specialty drugs. That’s 4 times a year. For someone working two jobs, caring for an elderly parent, and managing chronic pain - that’s not a form. That’s a second job.
And if you miss one deadline? No meds. No warning. Just a pharmacy telling you, ‘Sorry, your benefit expired.’
This isn’t assistance. It’s a compliance trap.
Katie O'Connell
December 17, 2025 AT 15:54It is imperative to underscore that the utilization of Modified Adjusted Gross Income (MAGI) as the primary metric for eligibility determination is both statistically robust and fiscally prudent, given its alignment with IRS-defined thresholds. However, the absence of standardized digital verification protocols across pharmaceutical entities introduces significant administrative inefficiencies, thereby exacerbating applicant attrition rates.
It is my professional opinion that a centralized, interoperable federal portal - analogous to the Healthcare Exchange - would mitigate the majority of documentation-related denials and enhance equity of access.
Jackie Petersen
December 19, 2025 AT 00:01Why should American taxpayers pay for rich drug companies to give out free medicine? They’re all just scam artists anyway. I bet they’re all immigrants who don’t even pay taxes and still want free pills.
My cousin’s brother got denied because he has a 2018 Toyota. That’s the problem. Too much compassion. We need borders and checks.
Annie Gardiner
December 20, 2025 AT 12:14Wait - so you’re saying the system is designed to make you fail? That’s actually kind of beautiful. Like a dark comedy written by Kafka and funded by Wall Street.
They want you to feel broken. They want you to beg. Then they pat themselves on the back for ‘helping.’
I’m not mad. I’m just… impressed by the artistry of the cruelty.
Kumar Shubhranshu
December 22, 2025 AT 10:25Why do you need a US doctor? My cousin in India gets the same drug for $10. You’re paying 100x because you let corporations own your healthcare.
Just order from Canada. Or India. Problem solved.
Kenny Pakade
December 22, 2025 AT 19:36Free medicine? No. This is socialism. We don’t need handouts. We need to stop letting foreigners get our drugs. And why are women always crying about this? Get a job. Or move to a real country.
brenda olvera
December 23, 2025 AT 18:10My grandma got her asthma inhaler for free last year. She cried when she got the letter. Said it was the first time in 10 years she didn’t have to choose between food and breath.
Don’t give up. Keep trying. There’s good people out there. And if you’re reading this - you’re not alone.
Love from Texas