Polypharmacy Risk Checklist: Identify Dangerous Medication Combinations Before It's Too Late
 Nov, 22 2025
Nov, 22 2025
Polypharmacy Risk Checker
Check if your medications could interact dangerously with common high-risk combinations. Always consult your healthcare provider before making changes to your medication regimen.
Every year, over 1.3 million people in the U.S. end up in the emergency room because of bad reactions to their medications. Most of them aren’t taking one dangerous drug-they’re taking five or more. This isn’t rare. One in three adults over 60 is on five or more prescriptions. And many of them don’t even realize their meds are working against each other.
Polypharmacy-taking five or more medications at once-isn’t always wrong. For someone with heart failure, diabetes, and arthritis, multiple drugs may be necessary. But when those drugs interact, the risks multiply fast. Each extra pill increases your chance of a serious drug interaction by nearly 40%. And those interactions don’t just cause nausea or dizziness. They can lead to falls, kidney failure, confusion, and even death.
What Makes a Medication Combination High-Risk?
Not all drug combinations are equally dangerous. Some are silent killers. The most common high-risk pairings show up again and again in emergency rooms and hospital records.
- Warfarin + cranberry juice: Warfarin thins your blood. Cranberry juice makes it thinner-too thin. This combo can cause internal bleeding without warning.
- Statins + grapefruit juice: Grapefruit blocks the enzyme that breaks down statins. That means your body gets too much of the drug. Result? Muscle breakdown (rhabdomyolysis), which can wreck your kidneys.
- Blood pressure meds + decongestants (like pseudoephedrine): Decongestants spike your blood pressure. If you’re already on meds to lower it, this can cause a sudden, dangerous rise-sometimes leading to stroke.
- Acetaminophen + oxycodone + prochlorperazine: This trio shows up too often in ER visits. Acetaminophen harms the liver. Oxycodone causes drowsiness. Prochlorperazine adds more sedation. Together, they overload your brain and liver.
- Benzodiazepines (like diazepam) + opioids: Both depress your breathing. Combined, they’re a leading cause of accidental overdose in older adults.
Even over-the-counter stuff can be risky. Antihistamines in sleep aids or cold medicines? They’re strong anticholinergics. For older adults, these can cause memory loss, confusion, and urinary retention. The Beers Criteria-updated in 2019-lists these as medications to avoid in seniors unless absolutely necessary.
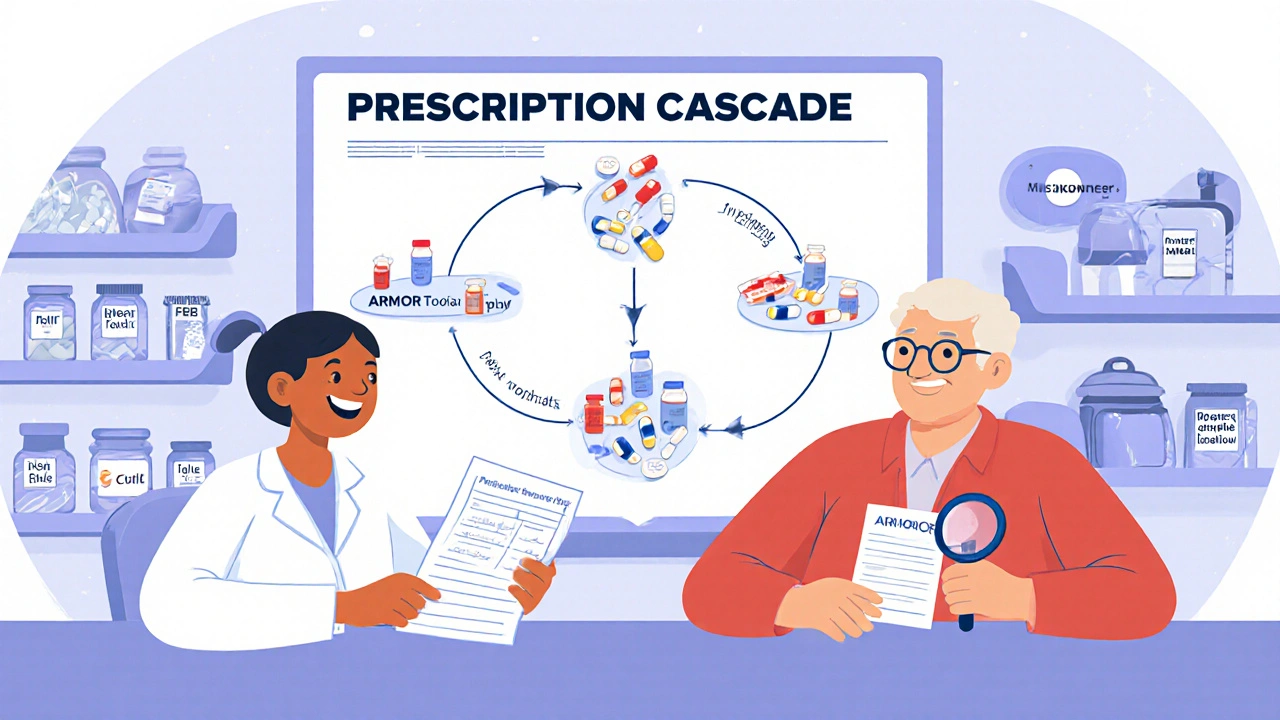
The Prescription Cascade: When One Drug Causes Another Problem
Here’s how it often starts: You take a painkiller for arthritis. It causes constipation. So your doctor prescribes a laxative. The laxative messes with your electrolytes, so you get dizzy. Now you’re on a blood pressure med to fix the dizziness. But that med makes you tired, so you take a sleep aid. And the cycle keeps going.
This is called a prescription cascade. It’s not malpractice. It’s systemic. Doctors see symptoms, not the whole picture. And if you’re seeing three different specialists, none of them may know what the others prescribed.
A study in Ohio found 67% of seniors were taking at least one medication that shouldn’t have been prescribed to them-often because it was meant to treat a side effect of another drug. One patient on Reddit shared how he ended up in the hospital after taking a decongestant with his blood pressure pill. He didn’t know they clashed. His doctor didn’t know he was taking it.
The Polypharmacy Risk Checklist: Your Action Plan
You don’t need to guess which meds are risky. Use this checklist every time you see a doctor or pharmacist.
- Make a full list: Write down every pill, patch, liquid, vitamin, herb, and supplement you take-even aspirin or melatonin. Include dosages and how often you take them.
- Bring it to every appointment: Don’t rely on memory. Don’t assume your doctor has the right file. Hand them the list. Ask: “Is any of this dangerous together?”
- Check for Beers Criteria flags: Look up the Beers Criteria list (available free from the American Geriatrics Society). If you’re over 65, ask your pharmacist: “Does any of my med fall under this?”
- Ask about food interactions: Grapefruit, cranberry, alcohol, and even dairy can interfere with meds. Don’t assume your doctor will mention it. Ask: “What should I avoid eating or drinking with this?”
- Question every new prescription: When a new drug is added, ask: “Why is this needed? What side effect is it fixing? Can we stop something else?”
- Use the ARMOR tool: Assess your meds. Review each one’s purpose. Minimize what’s unnecessary. Optimize dosages. Reassess every 3-6 months. This isn’t just for doctors-it’s a framework you can use yourself.
- Know your pharmacist: Pharmacists are trained to spot interactions. They see your full history. Ask for a free medication review. Many pharmacies offer it.
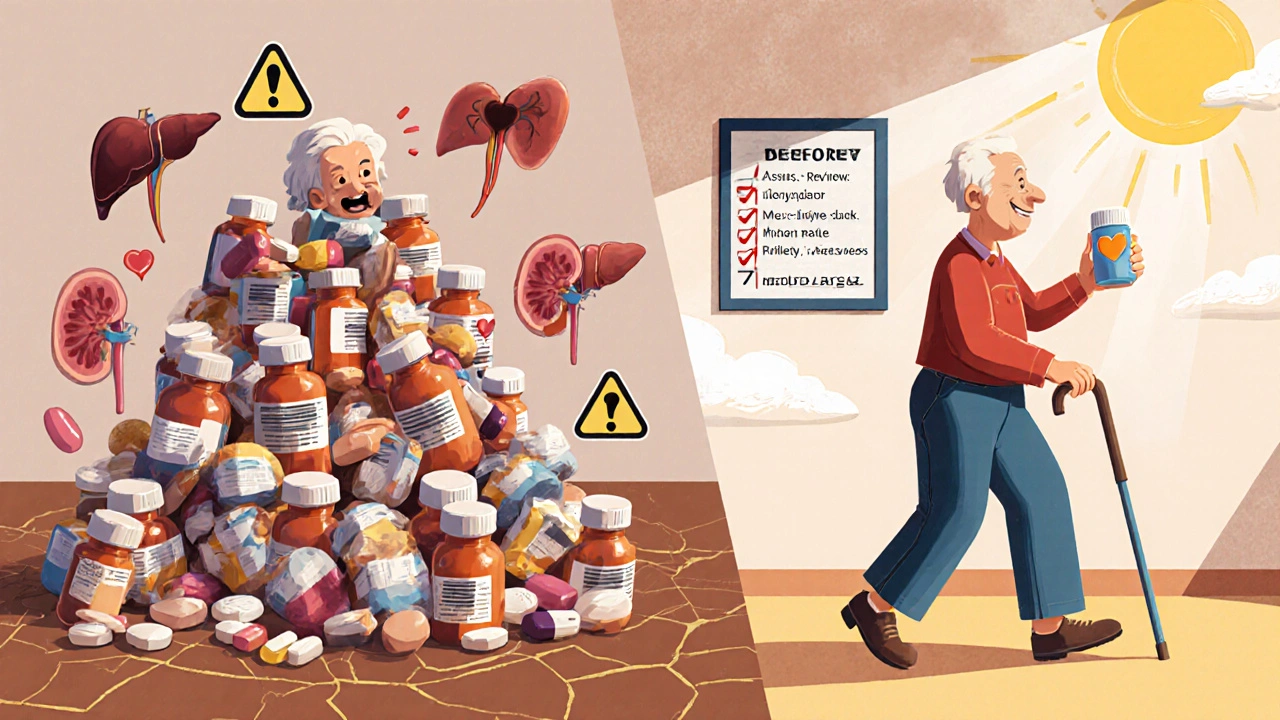
Who’s Most at Risk?
Polypharmacy isn’t equal across the board. Certain groups face much higher danger:
- People over 65: Your liver and kidneys don’t process drugs as well. Side effects hit harder and last longer.
- People with cancer: Nearly 61% of cancer patients take five or more meds before starting chemo. Many of those are supplements or OTC drugs they think are harmless.
- People seeing multiple specialists: A cardiologist, neurologist, and rheumatologist may each prescribe without knowing the others’ plans.
- People on Medicaid or Medicare: Higher rates of polypharmacy are linked to cost pressures and fragmented care.
And here’s the quiet truth: Many of these meds aren’t even working anymore. A 2023 study found that 40% of medications taken by cancer patients were inappropriate-either outdated, redundant, or causing more harm than good.
What Happens When You Reduce Your Meds?
People think taking fewer pills means getting worse. But often, the opposite is true.
A 72-year-old cancer patient on the CancerCare forum reduced her meds from 12 to 7 using the ARMOR method. Her energy improved. Her confusion cleared. Her falls stopped. She didn’t lose any cancer control.
Another study found that seniors who had one or more unnecessary meds stopped had a 30% lower risk of falling. Their balance got better. Their memory improved. Their quality of life went up.
Deprescribing isn’t about quitting meds. It’s about removing what’s not helping-or hurting. It’s a slow, careful process. Never stop a drug cold turkey. Work with your doctor. Taper slowly. Track how you feel.
Why Aren’t Doctors Doing More?
Electronic health records are supposed to warn doctors about bad combinations. But here’s the problem: 96% of those alerts get ignored.
Why? Alert fatigue. If your computer pings you 20 times a day with warnings-most of them unimportant-you stop paying attention. The system is broken.
Doctors are rushed. They have 15 minutes per patient. They’re not trained in pharmacology. And many don’t know the Beers Criteria or how to use the ARMOR tool.
The real solution? You. You have to be your own advocate. You have to ask the questions. You have to bring the list. You have to push back when something feels off.
What’s Next? The Future of Medication Safety
Researchers are building smarter tools. One new system uses AI to map out your entire medication history and predict which combinations are most likely to cause harm. Another uses smart pill bottles that track when you take your meds-and flag if you’re missing doses or doubling up.
Some clinics are starting to test genetic testing to see how you metabolize drugs. If your body breaks down a certain med slowly, you need a lower dose. That’s personalized medicine.
But none of that matters if you don’t start now. The World Health Organization’s 2023 goal is to cut severe medication harm by 50% by 2027. That won’t happen unless patients take control.
You don’t need to be a doctor. You just need to be informed. You don’t need to fight the system. You just need to ask the right questions.
What is polypharmacy and why is it dangerous?
Polypharmacy means taking five or more medications regularly. It’s dangerous because each additional drug increases the chance of harmful interactions by 39%. These interactions can cause falls, confusion, kidney damage, or even death. Many of these risks are preventable with a simple medication review.
Which medications should seniors avoid completely?
According to the Beers Criteria, seniors should avoid benzodiazepines (like diazepam), anticholinergic drugs (like diphenhydramine in sleep aids), and certain blood pressure meds like α1-blockers (e.g., doxazosin). These increase fall risk, confusion, and urinary problems. Even OTC cold meds with antihistamines can be dangerous.
Can grapefruit really make my statin dangerous?
Yes. Grapefruit blocks an enzyme in your liver (CYP3A4) that breaks down statins like atorvastatin and simvastatin. This causes too much of the drug to build up in your blood, raising your risk of rhabdomyolysis-a serious muscle breakdown that can damage your kidneys. Even one glass of grapefruit juice can have this effect for up to 72 hours.
How often should I get my meds reviewed?
Get a full medication review at least every 6 months-or anytime you see a new doctor, start a new drug, or feel different (dizzy, confused, tired). The WHO recommends this for older adults on multiple medications. Keep a written list and bring it to every visit.
Can I stop a medication on my own if I think it’s causing problems?
Never stop a prescription drug without talking to your doctor. Some meds, like blood pressure or antidepressants, can cause serious withdrawal symptoms if stopped suddenly. But you can ask: “Is this still necessary? Can we try reducing it?” Your pharmacist can help you prepare for that conversation.
What’s the ARMOR tool and how do I use it?
ARMOR stands for Assess, Review, Minimize, Optimize, Reassess. Start by listing all your meds. Review each one: Is it still needed? Is it causing side effects? Minimize by cutting unnecessary ones. Optimize doses. Reassess every few months. It’s a simple framework you can use yourself-no doctor needed to start.
Are supplements safe to take with my prescriptions?
No. Supplements aren’t regulated like drugs. St. John’s Wort can make antidepressants and birth control useless. Vitamin K can cancel out warfarin. Fish oil can increase bleeding risk with blood thinners. Always tell your doctor and pharmacist about every supplement you take-even if you think it’s harmless.
What to Do Today
Don’t wait for a crisis. Here’s your first step:
- Grab a piece of paper.
- Write down every pill, vitamin, herb, and OTC drug you’ve taken in the last 30 days.
- Call your pharmacy. Ask for a free medication review.
- Next time you see your doctor, hand them the list and say: “I’m worried some of these might be interacting. Can we go through them?”
Polypharmacy isn’t inevitable. It’s a system failure. But you don’t have to be its victim. With the right checklist and a little courage, you can take back control of your health.
Olanrewaju Jeph
November 23, 2025 AT 01:42Thank you for this incredibly clear and vital guide. I’ve seen too many elderly relatives on 10+ meds, none of whom ever got a full review. This checklist is exactly what we need - practical, actionable, and free of fearmongering. I’m printing this out for my dad’s next appointment.
Dalton Adams
November 23, 2025 AT 07:16Let’s be real - most doctors are glorified prescription clerks. They don’t know pharmacokinetics, they don’t read the Beers Criteria, and they’re too busy chasing EMR bonuses to care. I’ve had my own meds crossed three times because my PCP didn’t even check my pharmacy profile. The system is broken. AI tools? Cute. But until we stop incentivizing volume over safety, this will keep happening. 🤦♂️
Kane Ren
November 24, 2025 AT 19:30This is such a hopeful piece. I used to think reducing meds meant giving up on health - but seeing that 72-year-old’s story? That’s the kind of win we need more of. Small changes, big results. You’re not weak for wanting to feel better - you’re smart. Keep asking questions. Your body deserves better than a pill carousel.
Suresh Ramaiyan
November 26, 2025 AT 14:22It’s fascinating how medicine has become so fragmented. We treat symptoms like puzzle pieces, not symptoms of a system in distress. The prescription cascade isn’t just medical - it’s cultural. We’ve normalized taking pills for everything, even when the body is trying to tell us to slow down. Maybe the real question isn’t ‘what’s wrong with my meds?’ but ‘what’s wrong with how we think about health?’
Bryson Carroll
November 27, 2025 AT 15:22Everyone’s so worried about polypharmacy but nobody talks about how people just don’t take their meds right anyway. Half the people on this list are probably mixing up doses or skipping pills because they’re confused. So why are we blaming the doctors? Maybe the real issue is patient compliance. Or maybe people just don’t care enough to read the damn label. I’ve seen people take Tylenol with Vicodin and act shocked when their liver fails. It’s not the system. It’s the people.
Jennifer Shannon
November 28, 2025 AT 02:27Oh my goodness, this post? I cried. I really did. My mom’s on 14 medications - 7 of them for side effects of the others - and I’ve been too scared to say anything because I didn’t want to sound like I was accusing her doctors of being careless. But now? I’m printing this out. I’m making a color-coded chart. I’m calling her pharmacist tomorrow. And I’m telling her: ‘Mom, you don’t have to feel this tired all the time.’ I’m so glad someone finally said it out loud. 💙
Suzan Wanjiru
November 28, 2025 AT 04:57Biggest thing I learned: grapefruit juice isn’t just bad with statins - it’s dangerous with over 50 meds. I had no idea. I drink it every morning. I’m switching to orange juice today. Also - pharmacists are your secret weapon. I asked mine to do a review and she found three duplicates I didn’t even know I was taking. Free service. Do it.
Kezia Katherine Lewis
November 28, 2025 AT 08:44From a clinical pharmacy perspective: the ARMOR framework is underutilized but empirically validated. The Assess-Review-Minimize-Optimize-Reassess model aligns with the 2023 AGS guidelines and has demonstrated a 32% reduction in high-risk prescribing in community-based trials. The key is longitudinal reassessment - not one-off audits. Pharmacist-led deprescribing initiatives show the most sustainable outcomes when integrated into primary care workflows.
Henrik Stacke
November 29, 2025 AT 20:55My grandfather, God rest him, took 11 pills a day. He never complained - but he stopped laughing. He stopped walking to the garden. He stopped remembering my name. When we finally reduced his meds - just four - he smiled again. He asked me to read him the newspaper. That’s not medicine. That’s magic. Thank you for writing this. I’ll share it with everyone I know.
Manjistha Roy
November 30, 2025 AT 09:32This is exactly what I’ve been trying to tell my aunt for years - she’s on warfarin, and she drinks cranberry juice every day because ‘it’s healthy.’ I’ve shown her articles, I’ve called her doctor, I’ve even printed out the Beers Criteria. She still says, ‘But the TV says cranberry is good for your bladder!’ We need more public education - not just for seniors, but for their families too. This checklist? It’s a lifeline.
Jennifer Skolney
December 1, 2025 AT 08:04Just shared this with my mom and my sister. We’re all going to make our own med lists this weekend. I used to think supplements were ‘safe’ - now I know St. John’s Wort can wreck my antidepressants. 😳 I’m so grateful for this post. Let’s all be better advocates for ourselves and our loved ones. 💪❤️
JD Mette
December 3, 2025 AT 00:12I’ve been a caregiver for my mother with dementia for seven years. I didn’t realize until now that some of her ‘sleep aids’ were making her confusion worse. This post didn’t just inform me - it gave me permission to question. Thank you for not blaming the patient. That matters more than you know.
Demi-Louise Brown
December 3, 2025 AT 12:18Systemic failure. Not individual negligence. The burden of medication safety should not rest on patients. But until policy changes, this checklist is the most powerful tool we have. Distribute it widely. Print it on flyers. Hand it out at pharmacies. Knowledge is the only defense against a broken system.
Matthew Mahar
December 4, 2025 AT 11:07Wait so grapefruit juice and statins? I thought that was just a myth? I’ve been drinking it every day for 10 years. Oh god. I’m gonna go check my meds right now. Thanks for the wake up call.
Olanrewaju Jeph
December 5, 2025 AT 07:05JD Mette, you said you’re a caregiver - I want to say thank you. You’re not alone. And you’re doing more than you think. This isn’t just about meds - it’s about dignity. Keep asking. Keep showing up. That’s the real medicine.