Pregnancy Trimester-Specific Medication Risks: Safer Timing Strategies
 Feb, 12 2026
Feb, 12 2026
Trimester-Specific Medication Safety Calculator
Check if your medication is safe based on the trimester you're in. The calculator uses the latest medical guidelines to provide accurate risk assessments.
When you’re pregnant, taking any medication - even something as simple as an allergy pill or pain reliever - can feel like walking a tightrope. You need relief, but you’re terrified of harming your baby. The truth is, not all medications are risky at every stage of pregnancy. The timing of when you take a drug matters more than you might think. It’s not just about "avoiding drugs" - it’s about knowing when it’s safest to use them.
Why Timing Matters More Than You Realize
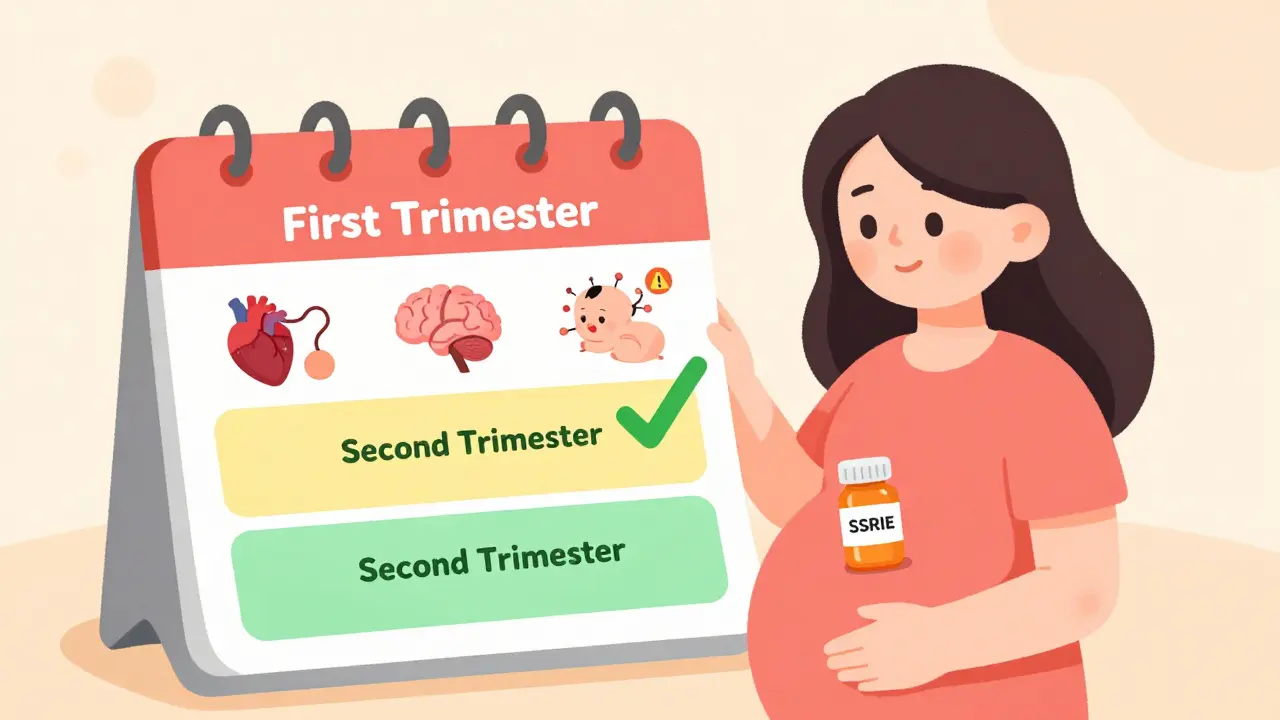
Most people think if a drug is dangerous in pregnancy, it’s dangerous all the time. That’s not true. The baby’s body changes dramatically in each trimester, and so do the risks. The first 12 weeks are when organs form. That’s the window for major birth defects. After that, the risks shift. By the third trimester, the baby’s organs are mostly built, but they’re still learning how to function. That’s when drugs can mess with breathing, heart rate, or even cause withdrawal after birth. This isn’t guesswork. It’s based on decades of research. After the thalidomide disaster in the 1960s - where babies were born with missing limbs because their mothers took the drug during a specific 10-day window - doctors realized: when you take a drug matters more than if you take it.First Trimester: The Critical Window for Birth Defects
Weeks 3 to 8 after fertilization - that’s the most sensitive time. It’s when the heart, brain, limbs, and face are forming. If a drug interferes during this period, it can cause structural defects. But here’s the twist: before day 20, if a medication causes harm, it usually leads to a miscarriage. If the pregnancy continues, the baby is likely fine. That’s called the "all-or-nothing" effect. Some drugs have clear, dangerous windows:- Isotretinoin (Accutane): Used for severe acne. If taken between days 21 and 55 after fertilization, it raises the risk of serious brain, heart, and ear defects by 50 times compared to the baseline. That’s why the FDA requires two negative pregnancy tests before you can even get a prescription - and monthly tests while you’re on it.
- Ondansetron (Zofran): Used for nausea. A 2019 study of 1.8 million pregnancies found a small increase in heart defects, but only if taken before week 10. After that, the risk drops to normal.
- ACE inhibitors (like lisinopril): Used for high blood pressure. These can cause kidney damage and skull defects if taken after week 8. That’s why doctors switch you to labetalol or methyldopa early in pregnancy.
Second Trimester: Less About Structure, More About Function
By week 13, most major organs are done forming. That’s good news. But the baby’s brain is still wiring itself. The lungs, liver, and kidneys are maturing. So while you won’t see a cleft palate or missing limb from a drug taken now, you might see problems later - like poor growth, learning delays, or abnormal brain activity. This is the safest window for most medications - but not all.- NSAIDs (ibuprofen, naproxen): Safe before week 20. After that, they can cause the ductus arteriosus (a vital blood vessel) to close too early. This can lead to heart problems in the newborn. Avoid them after 20 weeks.
- Metformin: Often used for PCOS or gestational diabetes. Many women stop it in the first trimester out of fear. But ACOG recommends continuing it throughout pregnancy. Stopping it can cause dangerous spikes in blood sugar - which are far riskier than the medication itself.

Third Trimester: The Newborn Withdrawal Risk
The baby’s body is almost ready for life outside the womb. But that means it’s also sensitive to how drugs affect its nervous system. If you’ve been taking certain medications daily for weeks, your baby’s body gets used to them. When you stop - or when the drug leaves the system after birth - withdrawal can happen. This is especially true for:- SSRIs (like sertraline, paroxetine): Used for depression and anxiety. In the third trimester, about 20-30% of babies exposed to SSRIs show signs of withdrawal: jitteriness, trouble feeding, fast breathing, or even seizures. The risk is highest with paroxetine. Sertraline has a much lower risk. A 2022 meta-analysis of 1.2 million pregnancies found paroxetine increased cardiac defect risk if taken during days 20-24 after fertilization - but that’s in the first trimester. The third-trimester risk is about withdrawal, not structure.
- Antidepressants and opioids: Both can cause neonatal abstinence syndrome (NAS). If you’re on opioids, your doctor should help you taper slowly before delivery.
Here’s the good news: if you’re on an SSRI and your mental health is stable, stopping abruptly can be more dangerous than continuing. A mother on Reddit (u/MamaMedSafety) shared how she successfully lowered her sertraline dose by 25% every two weeks starting at 34 weeks. Her second baby had no withdrawal symptoms - unlike her first, who was born in distress after she quit cold turkey at 36 weeks.
What’s Actually Safe?
Some medications have solid safety data across all trimesters:- Acetaminophen (Tylenol): Still the #1 choice for pain and fever. Over 24 studies involving 215,000 pregnancies show no link to developmental issues at standard doses (up to 3,000 mg/day). Avoid long-term high doses (over 3,500 mg/day for more than two weeks) - that’s where risks may start.
- Doxylamine/pyridoxine (Diclegis): The only FDA-approved nausea medication for pregnancy. Studies show no increase in birth defects, even in the first trimester.
- Labetalol: A blood pressure medication with no significant risk of malformations across all trimesters. Often used as a first-line option.
- Loratadine (Claritin): An antihistamine with a Category B rating. No proven risk in pregnancy. Yet many women are told to avoid all allergy meds in the first trimester - that’s outdated advice.
How to Navigate This Without Panic
The biggest problem isn’t the drugs - it’s the confusion. A 2023 survey of 1,200 pregnant people found 68% turned to social media for advice. And 42% got conflicting answers about the same medication. One doctor says "avoid ibuprofen entirely." Another says "it’s fine before 20 weeks." That’s not helpful. Here’s what actually works:- Know your dates. Most women use their last period to guess how far along they are. But the real clock starts at fertilization. If you’re told you’re 10 weeks pregnant, you’re likely 8 weeks post-fertilization. That changes everything. Ultrasound dating within 5 days of your exposure is critical for accurate risk assessment.
- Don’t stop meds without talking to your doctor. Stopping antidepressants, thyroid meds, or insulin can be more dangerous than the drug itself. Your condition matters as much as the drug.
- Use trusted resources. The CDC’s "Treating for Two" tool and MotherToBaby (run by experts at OTIS) offer free, science-backed guidance. They don’t rely on Reddit threads.
- Ask for a medication review. Bring your full list - prescriptions, OTCs, supplements - to your OB or midwife. Don’t assume they know what you’re taking.
The Future: Personalized Timing
Right now, we’re still using broad guidelines. But things are changing. The NIH just funded a project to build a trimester-specific risk calculator that factors in your genetics, how your body processes drugs, and exact gestational age. By 2028, we may be able to say: "Based on your DNA and when you conceived, this dose of sertraline is safe. That one isn’t." Until then, the best strategy is simple: don’t guess. Don’t panic. Get precise. Your baby’s development is a clock - and every drug has its own schedule. Knowing the timing isn’t just smart. It’s life-changing.Can I take ibuprofen during pregnancy?
Ibuprofen and other NSAIDs are generally safe before week 20. After that, they can cause the baby’s ductus arteriosus to close too early, leading to heart problems. They can also reduce amniotic fluid levels. For pain relief after week 20, use acetaminophen instead. Always check with your provider before taking any NSAID.
Is it safe to continue antidepressants during pregnancy?
For many people, yes. Untreated depression or anxiety can lead to poor prenatal care, preterm birth, or low birth weight. Sertraline (Zoloft) has the strongest safety record among SSRIs. If you’re stable on your current medication, stopping abruptly can be more harmful than continuing. Work with your OB and psychiatrist to adjust doses if needed - especially in the third trimester to reduce newborn withdrawal risk.
What should I do if I took a risky medication before knowing I was pregnant?
Don’t panic. The risk is often much lower than you think. Many medications have no proven risk, and some only cause issues during very narrow windows. Contact MotherToBaby (1-800-973-3864) or your OB. They’ll help you figure out exactly when you were exposed and whether it aligns with a known risk period. Most exposures don’t lead to birth defects - and ultrasound dating can confirm whether the baby is developing normally.
Are natural remedies safer than medications during pregnancy?
Not necessarily. Many herbal supplements and essential oils aren’t tested for safety in pregnancy. Some - like black cohosh or high-dose vitamin A - can be harmful. Just because something is "natural" doesn’t mean it’s safe. Always check with a provider before using any supplement, tea, or essential oil during pregnancy.
How do I know if my doctor is giving me up-to-date advice?
Ask them which guidelines they follow - ACOG, FDA PLLR, or MotherToBaby. If they rely on outdated letter categories (A, B, C, D, X), they may be using information from before 2015. Request access to the CDC’s "Treating for Two" tool or ask if they use Micromedex or Lexicomp, which have updated trimester-specific data. If they can’t point to a current source, consider seeking a second opinion from a maternal-fetal medicine specialist.
Neha Motiwala
February 13, 2026 AT 08:22Gloria Ricky
February 14, 2026 AT 09:46Stacie Willhite
February 16, 2026 AT 00:21Brad Ralph
February 16, 2026 AT 19:48christian jon
February 16, 2026 AT 23:53Suzette Smith
February 18, 2026 AT 16:55Autumn Frankart
February 19, 2026 AT 13:52Skilken Awe
February 19, 2026 AT 17:41andres az
February 20, 2026 AT 04:34Steve DESTIVELLE
February 21, 2026 AT 03:13Stephon Devereux
February 22, 2026 AT 19:55steve sunio
February 23, 2026 AT 11:22athmaja biju
February 23, 2026 AT 17:46Robert Petersen
February 24, 2026 AT 19:14Craig Staszak
February 25, 2026 AT 01:34