Prior Authorization: How Providers Secure Approval for Generic Medications
 Dec, 16 2025
Dec, 16 2025
When a doctor prescribes a generic medication, many assume it’s a simple step - low cost, widely available, and covered. But in today’s U.S. healthcare system, that’s often not the case. Even for a $5 generic pill, providers must navigate a maze of paperwork, electronic portals, and insurer rules just to get approval. This is prior authorization, and for generics, it’s more common - and more confusing - than most patients realize.
Why Do Insurers Require Prior Authorization for Generics?
It seems counterintuitive. Generics are cheaper than brand-name drugs. So why would insurers make providers jump through hoops to approve them?
The answer lies in how pharmacy benefit managers (PBMs) and insurers manage costs. They don’t just want to stop expensive drugs - they want to control which generic is used. For example, if there are five generic versions of omeprazole, the insurer may only cover one brand of generic, usually the one they’ve negotiated the lowest price with. If a doctor prescribes a different generic, even if it’s clinically identical, the insurer blocks it unless the provider proves why the preferred one won’t work.
According to the Academy of Managed Care Pharmacy, 28% of all prior authorization requests involve generic medications. Most of these aren’t about safety - they’re about cost-shifting. Common triggers include:
- Requesting a 90-day supply when the plan only allows 30 days without approval
- Using a generic for an off-label purpose (like using a proton pump inhibitor beyond 8 weeks)
- Switching between generic manufacturers because the patient had a reaction to one version
For providers, this isn’t about blocking care - it’s about following rules that change from one insurer to the next. A 2023 AMA survey found that 92.7% of physicians say prior authorization requirements have increased over the last five years. And for generics, the burden is growing faster than ever.
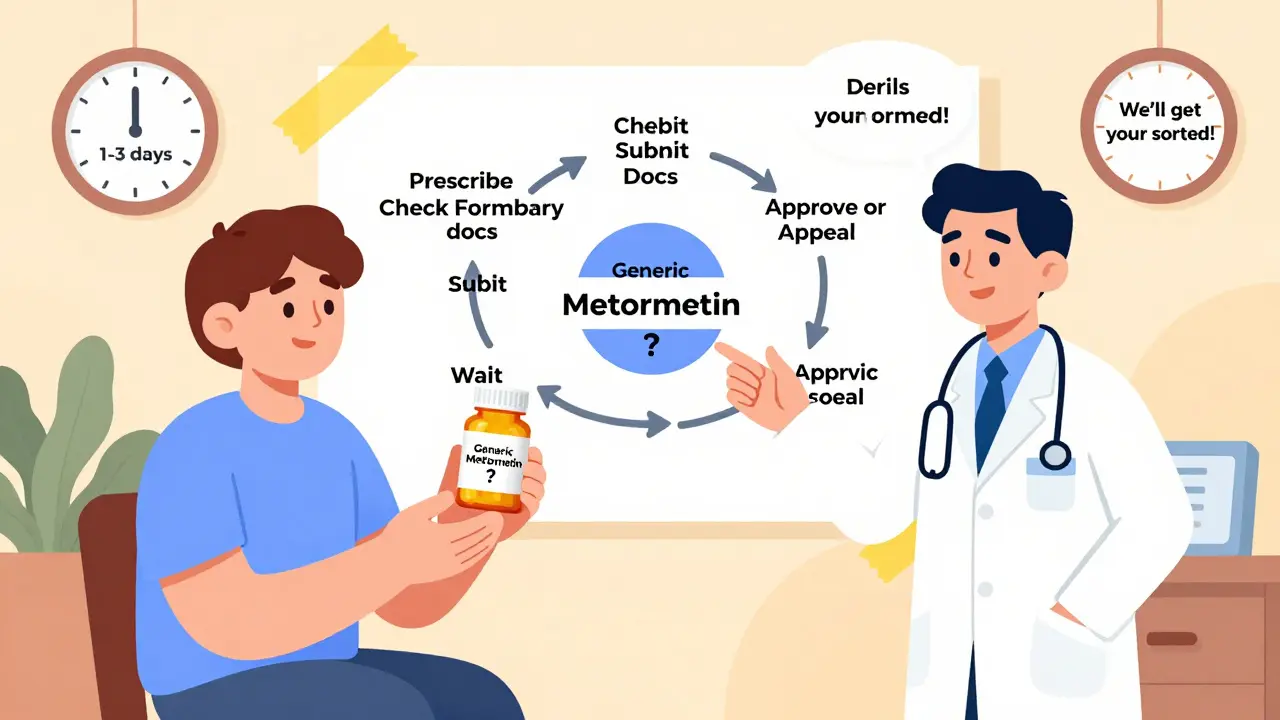
The Step-by-Step Process: How Providers Actually Get Approval
Securing approval for a generic isn’t one-size-fits-all. It depends on the payer - Medicaid, Medicare Part D, or a commercial insurer - and the specific drug. But the core steps are the same:
- Identify the requirement: Check the payer’s formulary. Is the prescribed generic on the preferred list? Is there a quantity or duration limit?
- Gather documentation: This is the most time-consuming part. You need clinical proof - chart notes, lab results, diagnostic reports. For example, if you’re requesting 12 weeks of omeprazole for Barrett’s esophagus, you must attach the endoscopy report showing intestinal metaplasia.
- Submit electronically: 78% of commercial insurers and 63% of Medicare Part D plans now require electronic submission through platforms like CoverMyMeds or Surescripts. Fax is still used by 22%, but it’s slower and more error-prone.
- Wait for response: Medicaid must respond within 24 hours for urgent cases and 14 days for standard ones. Commercial insurers typically take 5-10 business days. Auto-approval happens in 41% of cases when quantity limits aren’t exceeded and documentation is complete.
- Appeal if denied: If denied, providers must submit additional evidence - like proof of adverse reaction to the preferred generic - and reapply.
One provider on Reddit shared how they secured approval for omeprazole 40mg daily for 12 weeks by submitting the endoscopy report. It took two business days. Another, on Sermo, was denied for sitagliptin because the insurer demanded proof of three failed diabetes drugs - even though ADA guidelines say metformin intolerance alone is enough to switch. That’s the inconsistency providers face daily.
How Approval Times Differ Between Generics and Brand-Name Drugs
Here’s something many don’t realize: generics often get approved faster than brand-name drugs. Why? Because insurers have less to lose. Brand-name drugs cost hundreds of dollars per month - insurers want to ensure they’re truly necessary. Generics cost pennies. So if the clinical case is solid, the system often lets them through quicker.
GoodRx data from August 2024 shows:
- Generics: 1-3 business days average approval time
- Brand-name drugs: 3-7 business days average approval time
This speed gap exists because prior authorization for generics is usually about formulary compliance, not clinical risk. If the patient has a documented allergy to one generic version, or needs a specific formulation (like a dye-free pill for a child), the approval process is often streamlined - as long as the documentation is clear.
That’s why experienced practices use standardized templates. Capital Rx reports that providers using these templates see 32% faster approval times for generics. One template might include: patient name, drug name, dose, reason for deviation from preferred generic, supporting clinical evidence, and payer-specific codes.

What’s Different Across Insurance Types?
Not all insurers play by the same rules. The variation is staggering.
Here’s how prior authorization requirements stack up:
| Payer Type | Requires PA for Generics? | Typical Approval Time | Auto-Approval Rate |
|---|---|---|---|
| Medicaid (FFS) | 67% | 24 hrs (urgent), 14 days (standard) | 38% |
| Medicare Part D | 89% | 5-7 business days | 40% |
| Commercial Insurance | 93% | 5-10 business days | 41% |
Medicaid has federal mandates on turnaround times. Medicare Part D has new rules under the Improving Seniors’ Timely Access to Care Act: by January 2024, 90% of standard requests must be approved within 72 hours. Commercial insurers? No federal caps. Many still take 10+ days.
And here’s the kicker: 68% of physician practices report approval takes 1-3 days only if documentation is complete. If the payer asks for more info? That jumps to 7-14 days. That’s a week of patients going without meds.
Common Reasons for Denial - and How to Avoid Them
Denials for generic prior authorizations aren’t random. They follow patterns.
According to the AMA, the top three reasons for denial are:
- Lack of required documentation - 42%
- Failure to demonstrate medical necessity - 38%
- Failure to try the preferred generic first - 20%
Let’s break those down.
Lack of documentation: Providers forget to attach lab results, discharge summaries, or allergy records. A simple missing endoscopy report can derail a request for omeprazole.
Failure to demonstrate medical necessity: Just saying “the patient prefers this one” isn’t enough. You need clinical justification - e.g., “Patient developed rash with Teva’s generic metformin but tolerated Mylan’s version without issue.”
Failure to try preferred generic: Insurers often require a “step therapy” trial. If the preferred generic is Amlodipine 5mg from Mylan, and you prescribe Amlodipine 5mg from Teva, you must show why Mylan didn’t work - not just that the patient likes Teva better.
Pro tip: Keep a payer-specific checklist. One insurer might require a signed letter from the provider. Another might need a specific ICD-10 code. Write them down. Update them quarterly. Save time. Reduce denials.
What’s Changing in 2025 - And What It Means for Providers
The system is shifting - fast.
As of July 1, 2024, CMS mandated that Medicaid managed care organizations use standardized electronic prior authorization transactions. That’s expected to cut processing times by 25%. By 2026, McKinsey predicts 75% of generic prior authorizations will be auto-approved by AI systems, reducing wait times to under 24 hours.
Express Scripts reported a 40% increase in auto-approvals for generics in 2023. That’s because insurers are realizing: if the drug is generic, the quantity is within limits, and the patient has no history of misuse - why not just approve it?
But the AMA is pushing back. They’re lobbying for state laws that would eliminate prior authorization for generics that have been on the market for over five years and have multiple manufacturers. The argument? There’s no clinical reason to restrict them. The FDA considers them interchangeable. So why make providers waste hours?
Meanwhile, the Congressional Budget Office warns that if nothing changes, provider administrative costs tied to prior authorization could hit $1.2 billion by 2026. That’s not just time - it’s money. Staff hours. Burnout. Missed patient appointments.
How Providers Are Adapting - And What Works
Successful practices don’t wait for the system to fix itself. They build systems of their own.
- Dedicated staff: MGMA found that 78% of routine prior authorizations are handled by trained medical assistants under physician supervision.
- Electronic tools: CoverMyMeds, Surescripts, and other platforms reduce errors and speed up submission.
- Templates: Pre-written documentation for common scenarios (e.g., PPIs, statins, metformin) cuts approval time by a third.
- Payer relationships: Calling a payer rep to clarify a denial saves days. Many providers keep a list of direct contacts.
- Training: New providers need 2-3 weeks to get comfortable with the process. Don’t leave it to chance.
One clinic in Ohio reduced generic prior authorization denials by 60% in six months by assigning one MA to manage all PA requests, using templates, and submitting electronically. They now spend 10 fewer hours per week on paperwork.
That’s not just efficiency - it’s patient care. Because when a provider spends 16.1 hours a week on prior authorization, they’re not seeing patients. That’s the real cost.
What Patients Don’t Know - But Should
Most patients assume their doctor controls what medication they get. But in reality, the insurer often does.
A 2023 survey by the National Community Pharmacists Association found that 83% of pharmacists have had patients walk out because they couldn’t afford to pay out-of-pocket for a generic while waiting for approval. That’s not hypothetical. That’s happening every day.
Providers need to set expectations early. Say it plainly: “This generic needs approval from your insurance. It could take a few days. We’ll submit right away, but you might need to wait.” That honesty prevents frustration, missed doses, and lost trust.
And when possible, use alternatives. If a patient needs a generic but the insurer denies it, ask: Is there another generic on the formulary? Can we switch to a different class? Sometimes, the answer isn’t fighting the system - it’s working around it.
Prior authorization for generics isn’t going away. But it doesn’t have to be a black box. With the right tools, documentation, and strategy, providers can cut through the noise - and get patients the meds they need, faster.
Do all insurance plans require prior authorization for generic medications?
No, but most do. As of 2024, 93% of commercial insurance plans, 89% of Medicare Part D plans, and 67% of Medicaid fee-for-service programs require prior authorization for at least some generic medications. The requirement depends on the drug, the payer’s formulary, and whether there are multiple generic options available.
How long does it take to get prior authorization approved for a generic drug?
Approval times vary. Medicaid must respond within 24 hours for urgent requests and 14 days for standard ones. Commercial insurers typically take 5-10 business days. With electronic submissions and complete documentation, 41% of generic prior authorizations are auto-approved within 1-3 days. If additional information is needed, it can stretch to 7-14 days.
Why is prior authorization required for generics if they’re cheaper than brand-name drugs?
Even though generics are cheaper, insurers use prior authorization to control which specific generic is prescribed. If five generic versions of a drug exist, the insurer often negotiates a lower price with one manufacturer and wants providers to use that version. Prior authorization ensures patients don’t get a more expensive generic - even if it’s clinically identical.
Can a patient get a generic medication while waiting for prior authorization approval?
Sometimes, but not always. Many patients can’t afford to pay out-of-pocket for the generic while waiting. Some providers issue short-term bridge prescriptions or samples, but this isn’t always possible. About 56% of physicians report having to provide bridge prescriptions due to delays, which adds complexity and risk.
What documentation is needed to get prior authorization for a generic drug?
You need clinical proof that the requested generic is necessary. This includes chart notes, lab results, diagnostic reports (like endoscopies or MRIs), and documentation of adverse reactions to other generics. For example, if a patient had a rash with one generic version of metformin, you must show that in your submission to justify switching to another.
Are there any new laws or rules changing how prior authorization works for generics?
Yes. As of January 1, 2024, Medicare Advantage plans must approve 90% of prior authorization requests within 72 hours for standard cases and 24 hours for urgent ones. Also, as of July 1, 2024, Medicaid managed care plans must use standardized electronic prior authorization systems to reduce delays. The AMA is also pushing for state laws to eliminate prior authorization for generics that have been on the market for over five years and have multiple manufacturers.
Erik J
December 18, 2025 AT 02:45Just spent 45 minutes on CoverMyMeds for a $3 generic. The system auto-approved it 3 hours later. Meanwhile, my patient sat in the waiting room wondering why their blood pressure meds weren't ready. This isn't healthcare. It's bureaucratic obstacle course racing.
Steven Lavoie
December 19, 2025 AT 15:06The systemic absurdity here is not that generics require prior authorization-it's that we've normalized it. We treat pharmaceutical logistics like a game of whack-a-mole with insurance formularies, while clinicians are expected to be both doctors and compliance officers. The FDA deems these drugs interchangeable. The system does not. That's not efficiency. It's institutionalized dysfunction.
Brooks Beveridge
December 21, 2025 AT 04:02Hey everyone-just wanted to say I see you. I'm a PA in rural Kansas and I do this same dance every single day. I keep a printed checklist taped to my monitor: drug name, dose, reason for deviation, supporting docs, payer code. It’s saved me hours. And yeah, sometimes I cry in the supply closet after a 10-day denial. But we keep showing up. You're not alone. Keep using templates. Keep calling reps. Keep documenting. The system hates consistency-and that’s exactly why it works.
Also, if you haven’t tried Surescripts’ new auto-fill feature for PPIs? Do it. Game changer. 🙌
Meghan O'Shaughnessy
December 21, 2025 AT 07:08My mom got denied for her generic metformin because the insurer said she needed to try the other generic first. She’s 72. She’s had diabetes for 20 years. She’s never had a side effect. The ‘preferred’ generic gave her nausea. The system doesn’t care. It just cares about the contract between the PBM and the manufacturer.
Kaylee Esdale
December 23, 2025 AT 02:02Jody Patrick
December 23, 2025 AT 05:40Stop the nonsense. If it's FDA approved and generic, let it go. No forms. No calls. No delays. This is why people hate American healthcare. It's not the cost-it's the bullshit.
CAROL MUTISO
December 23, 2025 AT 11:44Oh honey. You think this is bad? Try getting a prior auth for a $12 generic antifungal cream when the insurer wants you to prove the patient’s athlete’s foot isn’t just ‘a bad case of dry skin.’ I once had to submit a photo of a fungal rash… taken with a patient’s phone… and signed by a notary. All for a cream that costs less than a subway token. We are not healing people. We are negotiating with a vending machine that only accepts Bitcoin and tears.
Martin Spedding
December 24, 2025 AT 08:10lol prior auth for generics? what a joke. 93% of insurancs require it? yeah right. probably 93% of docs just give up and write a brand name and bill it as 'off formulary'. the system is rigged. and the worst part? the patients dont even know they're being screwed. they just think their doc is an idiot. lol