Topical Medication Allergies: How to Spot Contact Dermatitis and Get Real Relief
 Jan, 24 2026
Jan, 24 2026
What Is Topical Medication Allergy?
You put on a cream for your rash. It burns. It itches worse. The redness spreads. You think, "This isn’t helping-it’s making it worse." You’re not wrong. That’s not a bad reaction to the medicine. That’s your body saying "this is an allergen." Topical medication allergies cause allergic contact dermatitis-a delayed immune response that shows up 24 to 72 hours after contact. It’s not irritation. It’s not infection. It’s your immune system mistaking a drug for a threat.
Unlike irritant contact dermatitis-which happens when a substance like soap or bleach burns your skin-this is an allergic reaction. It only happens after you’ve been exposed to the allergen before. Your body remembers it. Next time you touch it, your T-cells sound the alarm. The result? Red, blistered, peeling, intensely itchy skin that looks like it’s been burned.
It’s more common than you think. About 1 in 6 people who get patch tested for skin rashes turn out to be allergic to something in their topical meds. And the most common culprits? Antibiotics, steroids, numbing agents, and painkillers-all things you’d assume are safe to put on your skin.
Top 5 Culprits Behind Medication-Induced Rashes
Not all topical drugs are created equal when it comes to triggering allergies. Some are far more likely to cause problems. Here are the five most common offenders, based on real patch test data from North American and European clinics:
- Neomycin - Found in over-the-counter antibiotic ointments like Neosporin. Positive in nearly 1 in 10 patch tests. It’s in everything: wound creams, eye drops, even some hearing aid solutions.
- Bacitracin - Often paired with neomycin. Alone, it’s less common, but still triggers reactions in about 7.5% of allergic patients.
- Hydrocortisone and other corticosteroids - The irony? The very drugs used to treat rashes can cause them. About 1 in 50 people using topical steroids develop an allergy to them. This is especially common in eczema patients who’ve used steroid creams for years.
- Benzocaine - A local anesthetic found in teething gels, hemorrhoid creams, and sunburn sprays. It’s sneaky because it’s in so many non-prescription products.
- Ketoprofen - A topical NSAID used for muscle pain. It’s a strong allergen, especially in Europe, where it’s more widely used than in the U.S.
Here’s the kicker: you might not even realize you’re using these. Many patients think "I only use my prescription cream," but they’re also rubbing on hand sanitizer, diaper rash ointment, or even aloe vera gel that contains benzocaine or fragrance. The allergen hides in plain sight.
How Doctors Diagnose It (And Why Most Miss It)
Most doctors look at a rash and think: "Eczema flare. More steroid cream." They don’t think, "Could the treatment be the problem?" That’s why 40 to 60% of these allergies go undiagnosed at first.
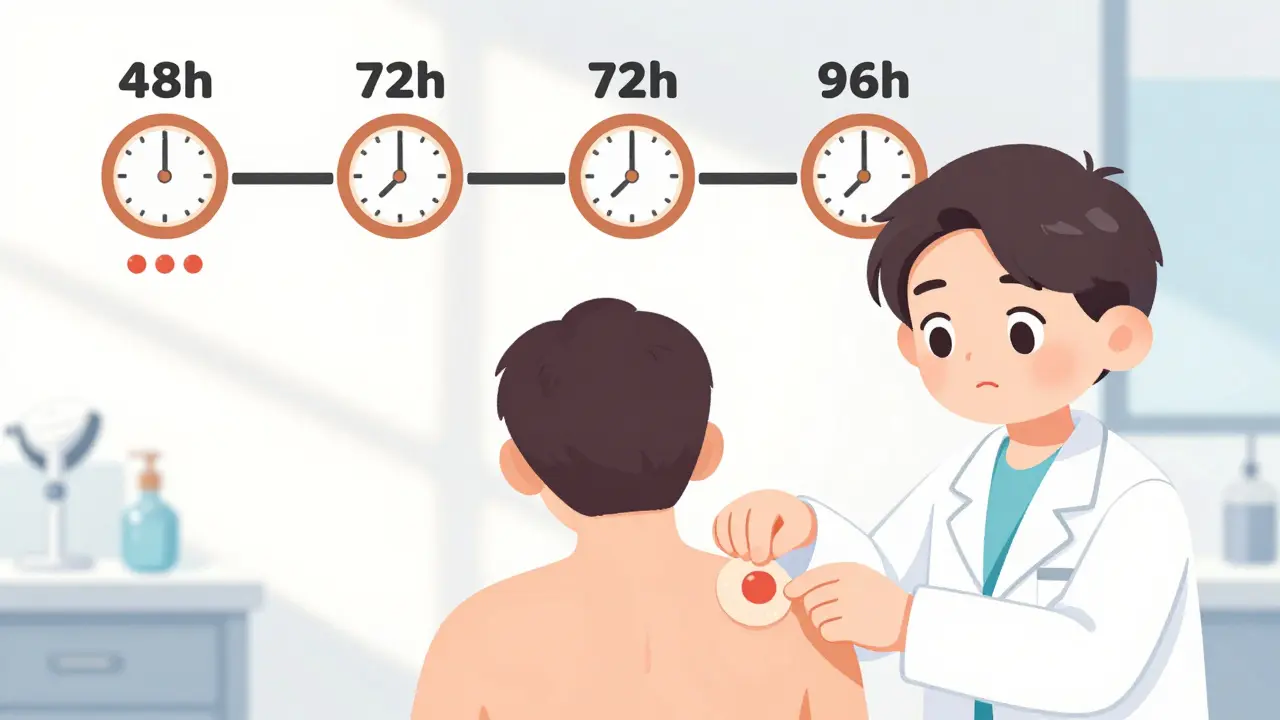
Here’s how it’s actually diagnosed: patch testing. It’s not a skin prick. It’s not a blood test. You have small discs containing suspected allergens taped to your back for 48 hours. Then, you come back at 72 hours and again at 96 hours. The doctor looks for tiny red bumps or blisters under each patch. That’s a positive reaction.
Why wait so long? Because this is a Type IV hypersensitivity reaction-it takes days for your immune cells to react. A skin prick test (used for peanut or bee sting allergies) won’t catch this. Only patch testing works.
And here’s the truth: if you’ve had a rash that won’t go away after using the same cream for weeks, or if your skin gets worse after applying treatment, ask for patch testing. It’s the only way to know for sure.
Treatment: Stop the Allergen, Then Soothe the Skin
The single most important step? Stop using the allergen. No cream, no spray, no ointment that contains the trigger. That’s it. That’s 89% of the battle.
Once you’ve identified the culprit-say, neomycin or hydrocortisone-you need to avoid it completely. That means checking every product label. Even "natural" or "hypoallergenic" products can contain hidden allergens. The American Contact Dermatitis Society has a free app that lets you scan product barcodes to check for 3,500+ allergens. Use it.
For active rash treatment:
- Mild cases: Over-the-counter 1% hydrocortisone can help-but only if you’re not allergic to it. If your rash flares after using it, stop immediately.
- Moderate to severe: Doctors prescribe mid- to high-potency steroids like triamcinolone 0.1% or clobetasol 0.05%. But avoid these on your face, eyelids, or groin. Use desonide instead-it’s weaker but safer for thin skin.
- Large areas (over 20% of body): Oral prednisone. Typically 40-60 mg daily for 2-3 weeks, then slowly tapered. Most people feel relief within 12-24 hours.
- Face or sensitive areas: Calcineurin inhibitors like pimecrolimus (Elidel) or tacrolimus (Protopic). These aren’t steroids. They don’t cause thinning skin. They work for about 65% of patients, though they can burn at first. That burning fades in a few days.
And yes, you can use tacrolimus even if you’re allergic to steroids. It’s a different mechanism. Many patients who thought they "couldn’t use anything" find relief here.
The Steroid Paradox: When the Cure Makes It Worse
Think about this: You have eczema. Your doctor prescribes hydrocortisone. You use it daily for months. Your skin clears. Then, one day, it comes back worse. Redder. Hotter. Burning. You think you’re getting resistant. But you’re not. You’re allergic.
Topical corticosteroid allergy happens in 0.5% to 2.2% of users. That sounds small, but multiply that by millions of users-and you’ve got tens of thousands of people being misdiagnosed every year. They’re told to use stronger steroids. Their skin thins. They get stretch marks. Their rash spreads. They feel like they’re failing.
Here’s the fix: Steroids are grouped into six categories based on chemical structure. If you’re allergic to group A (like hydrocortisone), you can usually use group B (triamcinolone) or group D (methylprednisolone aceponate) safely. That’s a 65% reduction in treatment limitations-if you know the groups.
Ask your dermatologist: "Which group is my steroid in?" If you’re allergic to one, they can switch you to a safe one without losing control of your condition.
What to Do If You Suspect a Topical Allergy
Here’s your step-by-step action plan:
- Stop all new topicals. Even if they’re "natural" or "prescribed by a friend."
- Write down everything you’ve applied to the affected area in the last 4 weeks. Include soaps, lotions, sunscreens, shampoos, and even diaper creams.
- Take photos. Document how the rash changes day by day.
- Go to a dermatologist who does patch testing. Not every dermatologist offers it. Call ahead. Ask: "Do you perform patch testing for topical medication allergies?"
- Bring all your products to the appointment. Thirty percent of allergens are found in non-prescription items you don’t think count as "medication."
- Once diagnosed, use the ACDS app or a similar tool to scan products. Avoid the allergen like poison.
Don’t wait. The longer you keep using the allergen, the more your skin barrier breaks down. That makes future reactions worse and harder to treat.

Real Stories: What Patients Say After Diagnosis
On Reddit, one woman wrote: "I used hydrocortisone for 5 years for my eczema. When it stopped working, I switched to stronger steroids. My face started peeling. I thought I had rosacea. I spent $2,000 on treatments. Then I got patch tested. Turns out, I was allergic to the steroid I’d been using since I was 12. I cried for an hour. Then I felt free."
A nurse from Texas shared: "I kept getting rashes on my hands. I thought it was from washing too much. Then I realized I was applying antibiotic ointment every time I got a cut. Neomycin. I stopped. The rash vanished in 10 days. No meds needed."
On RealSelf, 82% of people using tacrolimus for steroid allergies say they saw "significant improvement" within two weeks. The trade-off? A burning feeling at first. But most say: "Worth it."
And here’s the hard truth: 74% of people with these allergies see 3 or more doctors before getting the right diagnosis. They’re told they have psoriasis. Fungal infection. Stress rash. They’re prescribed antibiotics, antifungals, immunosuppressants. Nothing works. They lose hope.
The Future: Better Tests, Fewer Mistakes
Things are changing. In 2023, the European Society of Contact Dermatitis introduced a new diagnostic tool called the Topical Medication Allergy Score. It uses 12 specific clues-like rash location, timing after application, and past steroid use-to boost diagnosis accuracy from 65% to 89%.
Researchers at Johns Hopkins found that diluting topical medications 10 times before patch testing cuts false negatives by more than half. That’s huge for people with broken skin barriers who used to test negative even when allergic.
And the NIH just funded $4.7 million to develop a blood test that could predict who’s at risk for these allergies before they ever use a cream. Imagine never having to suffer through a rash just because you used a common ointment.
Bottom Line: It’s Not Your Skin. It’s the Medicine.
If your skin gets worse after applying a treatment, don’t blame yourself. Don’t assume it’s not working. Don’t reach for a stronger version. That’s the trap.
Topical medication allergies are real, common, and often missed. But they’re fixable. You don’t need to live with a rash that won’t heal. You don’t need to try 10 different creams. You just need to know what’s causing it-and stop using it.
Take control. Write down everything on your skin. Get patch tested. Avoid the trigger. Your skin will thank you.
Can you be allergic to hydrocortisone cream?
Yes. Hydrocortisone is one of the most common causes of topical medication allergies. It’s in many over-the-counter creams and even some prescription formulas. If your rash gets worse after using it, or if you develop redness, blistering, or peeling where you applied it, you may be allergic. Patch testing is the only way to confirm it.
How long does contact dermatitis take to heal?
Once you stop the allergen, itching usually improves within 48 to 72 hours. Full healing takes 2 to 4 weeks, depending on severity. If you keep using the allergen, the rash won’t go away-even with steroids. Avoidance is the cure.
Can I use Neosporin if I have a skin allergy?
Probably not. Neosporin contains neomycin and bacitracin-two of the top five allergens in patch testing. Nearly 1 in 10 people who get tested react to neomycin. Even if you’ve used it before without issue, you can develop an allergy over time. Use a plain petroleum jelly or a product labeled "neomycin-free" instead.
Are there steroid-free options for eczema?
Yes. Topical calcineurin inhibitors like pimecrolimus (Elidel) and tacrolimus (Protopic) are steroid-free and approved for eczema. They’re especially useful on the face, neck, and folds of skin. They work well for allergic contact dermatitis too, even if you’re allergic to steroids. Some people experience burning at first, but it fades.
Why don’t doctors test for this more often?
Because most doctors aren’t trained to suspect it. They see a rash and assume it’s eczema, psoriasis, or infection. They don’t think the treatment could be the cause. It’s a blind spot. But awareness is growing. Patch testing is now recommended by the American Contact Dermatitis Society for anyone with a chronic, treatment-resistant rash.
Can I get patch testing done without a referral?
In most cases, yes-but you’ll need to find a dermatologist or allergist who offers it. Not all do. Call ahead and ask: "Do you perform patch testing for topical medication allergies?" Some clinics require a referral, but many accept self-referrals, especially if you’ve had a rash for more than 6 weeks.
TONY ADAMS
January 25, 2026 AT 14:39George Rahn
January 26, 2026 AT 16:55Napoleon Huere
January 27, 2026 AT 15:48Uche Okoro
January 28, 2026 AT 18:55shivam utkresth
January 29, 2026 AT 05:43Kipper Pickens
January 30, 2026 AT 11:20Aurelie L.
January 31, 2026 AT 08:29Joanna Domżalska
February 1, 2026 AT 13:18Josh josh
February 2, 2026 AT 19:32bella nash
February 3, 2026 AT 03:26Curtis Younker
February 4, 2026 AT 17:45Ryan W
February 4, 2026 AT 18:27Renia Pyles
February 5, 2026 AT 04:37